Is there a connection between fibromyalgia (FM) and sleep disturbance? Let’s take a look!
FM is a condition that causes widespread pain and stiffness in muscles and joints. Patients with FM often experience chronic daytime fatigue and some type of sleep problems like getting to sleep, staying asleep, and/or feeling restored in the morning upon waking. The National Institutes of Health estimates between 80-90% of those diagnosed with FM are middle-aged women, although it can affect men and happen at any age. As little as 10-20 years ago, it was hard to find a doctor who “believed” in FM, and it was common for the patient to be told that their pain “was all in their head.” FM has now been studied to the point that we know it is a real condition, and it affects between 2-6% of the general population around the world.
It is well established that sleep disturbance frequently occurs after surgery, which usually normalizes as time passes. One study used a group of healthy women who were deprived of sleep (particularly slow wave sleep) for three days to see if there was a link between sleep disturbance and pain. Results confirmed that the women experienced a decrease in pain tolerance and increased levels of discomfort and fatigue after three days—the same symptoms found among FM sufferers!
Fibromyalgia may have NO known cause, or it can be triggered by other conditions such as repetitive stress injuries, car crash injuries, and other forms of trauma. FM also appears to run in families though it’s still NOT clear if this is a true genetic link or caused by shared environmental factors. Some feel FM is a rheumatoid condition, and though FM is NOT a true form of arthritis, it has been found that people with arthritis are more likely to have FM.
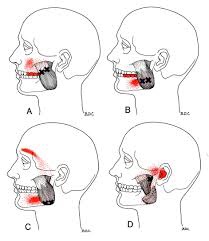
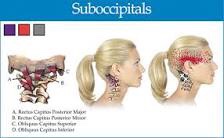
FM sufferers frequently suffer from conditions such as irritable bowel syndrome, chronic fatigue syndrome, migraine headaches, arthritis, lupus, and major depressive disorders. Approximately 20% of FM patients have depression and/or anxiety disorders, and a link between chronic pain and depression exists and seems to play a role in people’s perception of pain.
Because conditions such as sleep apnea can result in symptoms similar to FM, it’s recommended that patients suspected of FM keep a sleep/sleepiness diary in order to rule out sleep apnea as a cause for their condition.
There are many “tips” for improving sleep quality, which we will dive into next month, as these may prove VERY HELPFUL in the management of FM!
If you, a friend or family member requires care for Fibromyalgia, we sincerely appreciate the trust and confidence shown by choosing our services!