Temporomandibular Disorder (TMD) is a term used to describe a group problems that cause pain in the temporomandibular joint, also called the TMJ. These problems can arise from the muscles around the joint, the disc within the joint or the bony portion of the joint itself. Imbalances between the muscles that open and close your jaw are the most common culprit.

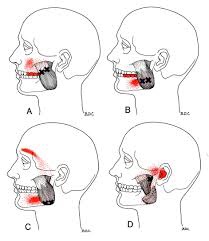
Up to 25% of the population will suffer with TMD symptoms. Most patients are 20-50 years old and the condition is 2-3 times more common in females. Typical symptoms include: jaw clicking, limited mouth opening, possible jaw locking and pain. Chewing and eating usually make your symptoms more noticeable. TMD pain is generally described as an “ache” located in front of your ear canal but may also refer to other areas of your face, head, neck and shoulders. TMD patients often suffer from headaches.
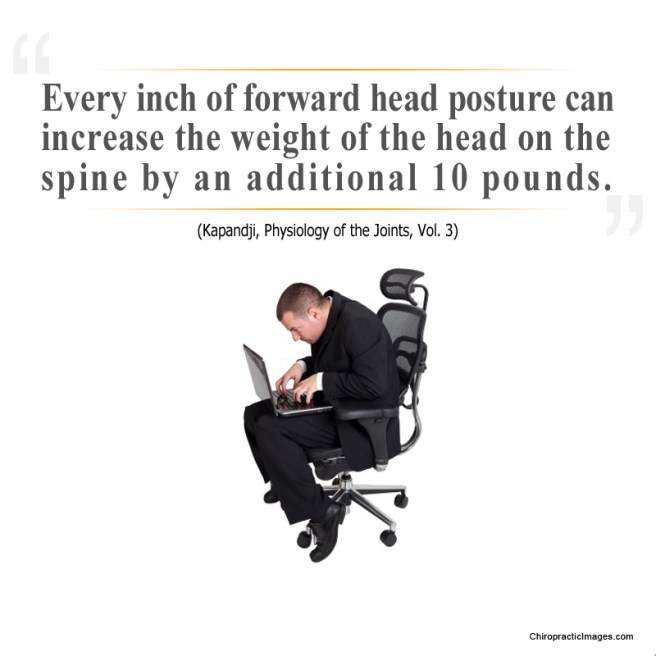
TMD is more common in people who clench their jaw or grind their teeth, especially at night. Bad posture and emotional stress are contributors to this problem. You are three times more likely to suffer with TMD if you have been involved in a “whiplash” accident.
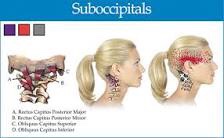
Conservative treatments, like those provided by our office, have been shown to be as effective as any surgery for most patients with TMD. Treatment is simple, focusing on “massaging” tightness out of the jaw muscles, restoring movement to any restricted joints (including your neck and upper back), and prescribing exercises to improve flexibility.
You should avoid aggravating activities like chewing gum or eating “rubbery” foods. Limit excessive talking. A custom fitted mouth guard may be prescribed to help minimize grinding & clenching and promote relaxation of your jaw muscles at night. Patients with night-time symptoms should avoid stressful activity before bedtime and try to sleep in a “neutral” position. In some cases, stress management techniques, like biofeedback, can assist you in learning how to relax your jaw muscles.