The levator scapula is a muscle located in your neck. It originates on the transverse processes of C1-C4 vertebrae. It inserts on the superior part of the medial border of the scapula. This muscle acts to elevate the scapula and rotate the glenoid fossa downward. At the cervical attachment it acts to rotate the neck to the same side and assists extension. Trigger points will refer pain into the angle of the neck with spillover into the scapula. When this muscle is tight due to trigger points it will restrict neck rotation causing the classic stiff neck. With a forward head position this muscle often becomes stretched and over worked.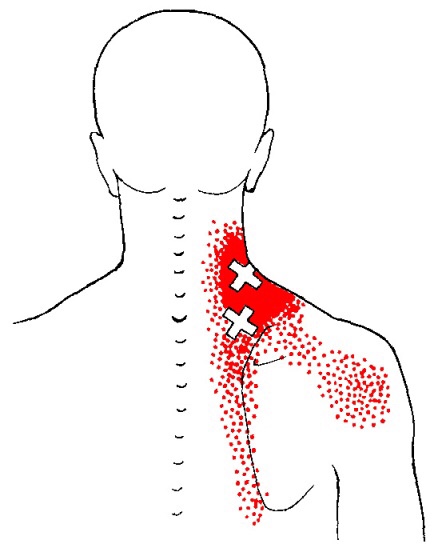
Shoulder Pain
A treatment with Bryan Cobb RMT.
Session Description
A treatment with Bryan is very user friendly. And, no, you don’t have to remove any clothing. However, bringing a t-shirt and a pair of shorts or sweats is recommended.
The first time you come for a treatment you will be asked to fill out a Client History form. Bryan will go over the information you provide, asking for more detail and discussing the type of pain you are having and its location.
The treatment itself involves locating the Trigger Points in the muscle or soft tissue and applying a deep focused pressure to the Point. This will reproduce the pain and the referral pattern that is characteristic of that pain.
The treatment will be uncomfortable at first, but as the Trigger Points release, the pain will decrease. The pressure will always be adjusted to your tolerance level. If, at any time, you feel too uncomfortable you can ask Bryan to ease off a bit.
Depending on your specific problem, Bryan may also use some stretching and / or range-of-motion techniques, as needed.
After treatment, it is usually recommended that the client apply moist heat to the area treated.
What the Heck Is a Trigger Point?
By Bryan Cobb, Advanced Remedial Massage Therapist
What is a Trigger Point?
Trigger Points (TP’s) are defined as a “hyper-irritable spot within a taut band of skeletal muscle. The spot is painful on compression and can evoke characteristic referred pain and autonomic phenomena.”1
Put into plain language, a TP is a painful knot in muscle tissue that can refer pain to other areas of the body. You have probably felt the characteristic achy pain and stiffness that TP’s produce, at some time in your life.
TP’s were first brought to the attention of the medical world by Dr. Janet G. Travell. Dr. Travell, physician to President John F. Kennedy, is the acknowledged Mother of Myofascial Trigger Points. In fact, “Trigger Point massage, the most effective modality used by massage therapists for the relief of pain, is based almost entirely on Dr. Travell’s insights.”2 Dr. Travell’s partner in her research was Dr. David G. Simons, a research scientist and aerospace physician.
Trigger Points are very common. In fact, Travell and Simons state that TP’s are responsible for, or associated with, 75% of pain complaints or conditions.1 With this kind of prevalence, it’s no wonder that TP’s are often referred to as the “scourge of mankind”.
Trigger Points can produce a wide variety of pain complaints. Some of the most common are migraine headaches, back pain, and pain and tingling into the extremities. They are usually responsible for most cases of achy deep pain that is hard to localize.
A TP will refer pain in a predictable pattern, based on its location in a given muscle. Also, since these spots are bundles of contracted muscle fibres, they can cause stiffness and a decreased range of motion. Chronic conditions with many TP’s can also cause general fatigue and malaise, as well as muscle weakness.
Trigger Points are remarkably easy to get, but the most common causes are
•
TP’s (black dots) can refer pain to other areas (red)

Sudden overload of a muscle
• Poor posture
• Chronic frozen posture (e.g., from a desk job), and
• Repetitive strain
Once in place, a TP can remain there for the remainder of your life unless an intervention takes place.
Trigger Points Not Well Known
With thousands of people dealing with chronic pain, and with TP’s being responsible for — or associated with — a high percentage of chronic pain, it is very disappointing to find that a large portion of doctors and other health care practitioners don’t know about TP’s and their symptoms.
Scientific research on TP’s dates back to the 1700’s. There are numerous medical texts and papers written on the subject.
But, it still has been largely overlooked by the health care field. This has led to needless frustration and suffering, as well as thousands of lost work hours and a poorer quality of life.
How Are Trigger Points Treated?
As nasty and troublesome as TP’s are, the treatment for them is surely straight-forward. A skilled practitioner will assess the individual’s pain complaint to determine the most likely location of the TP’s and then apply one of several therapeutic modalities, the most effective of which is a massage technique called “ischemic compression”.
Basically, the therapist will apply a firm, steady pressure to the TP, strong enough to reproduce the symptoms. The pressure will remain until the tissue softens and then the pressure will increase appropriately until the next barrier is felt. This pressure is continued until the referral pain has subsided and the TP is released. (Note: a full release of TP’s could take several sessions.)
Other effective modalities include dry needling (needle placed into the belly of the TP) or wet needling (injection into the TP). The use of moist heat and stretching prove effective, as well. The best practitioners for TP release are Massage Therapists, Physiotherapists, and Athletic Therapists. An educated individual can also apply ischemic compression to themselves, but should start out seeing one of the above therapists to become familiar with
the modality and how to apply pressure safely.
1 Simons, D.G., Travell, D.G., & Simons, L.S. Travell and Simons’ Myofascial Pain and Dysfunction: the Trigger Point Manual.
Vol. 1. 2nd ed. Lippincott, Williams, and Wilkins, 1999.
2http://www.muscletherapyworks.com/MTW%20Biography%20T%20&%20S%2001.htm
Trigger points in the deltoid muscle
The deltoid is the main muscle that makes up the shoulder. It originates on the clavicle, acromion, and spine of the scapula. It inserts on the deltoid tuberosity of the humerus. The deltoid acts at the shoulder to produce abduction, and assist with flexion and extension. The deltoid is especially prone to developing trigger points. These posterior style will refer pain into the anterior and lateral shoulder. Trigger points in the posterior delt will refer pain into the posterior shoulder with spillover down the lateral arm.
Help For Those Stuck At A Desk All Day
Desk workers should periodically perform the “Brugger relief position” to help maintain good sitting posture.
Here’s how to do it:
- Position your body at the chair’s edge, feet pointed outward. Weight should be on your legs and your abdomen should be relaxed.
- Tilt your pelvis forward, lift your sternum, arch your back, drop your arms, and roll out your palms while squeezing your shoulders together.
- Take a few deep cleansing breaths.
Learn more about proper workstation ergonomics in this video.
A Modern Spine Ailment
Some great information from Spine-Health.com and Dr. Steven Shoshany DC
Text neck is the term used to describe the neck pain and damage sustained from looking down at your cell phone, tablet, or other wireless devices too frequently and for too long.
Using a mobile device often can lead to poor posture and symptoms of text neck.
Watch: Text Neck Treatment Video<spanclass=”div-video-link”></spanclass=”div-video-link”>
And it seems increasingly common. Recently, a patient came in to my practice complaining of severe upper back pain. He woke up and was experiencing severe, acute, upper back muscle strain. I told him I believe the pain is due to the hours he was spending hunched over his cell phone. Diagnosis: Text neck.
Of course, this posture of bending your neck to look down does not occur only when texting. For years, we’ve all looked down to read. The problem with texting is that it adds one more activity that causes us to look down—and people tend to do it for much longer periods. It is especially concerning because young, growing children could possibly cause permanent damage to their cervical spines that could lead to lifelong neck pain.
See Cervical Spine Anatomy and Neck Pain
What are the symptoms associated with text neck?
Text neck most commonly causes neck pain and soreness. In addition, looking down at your cell phone too much each day can lead to:
-
- Upper back pain ranging from a chronic, nagging pain to sharp, severe upper back muscle spasms.
- Shoulder pain and tightness, possibly resulting in painful shoulder muscle spasm.
- If a cervical nerve becomes pinched, pain and possibly neurological symptoms can radiate down your arm and into your hand.
See What Is Cervical Radiculopathy?
I believe, as some studies suggest, text neck may possibly lead to chronic problems due to early onset of arthritis in the neck.
See Facet Joint Osteoarthritis
How common is text neck?
A recent study shows that 79% of the population between the ages 18 and 44 have their cell phones with them almost all the time—with only 2 hours of their waking day spent without their cell phone on hand.1
How is text neck treated?
First, prevention is key. Here are several pieces of advice for preventing the development or advancement of text neck:
-
- Hold your cell phone at eye level as much as possible. The same holds true for all screens—laptops and tablets should also be positioned so the screen is at eye level and you don’t have to bend your head forward or look down to view it.
See Ten Tips for Improving Posture and Ergonomics
-
- Take frequent breaks from your phone and laptop throughout the day. For example, set a timer or alarm that reminds you to get up and walk around every 20 to 30 minutes.
- If you work in an office, make sure your screen is set up so that when you look at it you are looking forward, with your head positioned squarely in line with your shoulders and spine.
See Ergonomics of the Office and Workplace: An Overview
The bottom line is to avoid looking down with your head bent forward for extended periods throughout the day. Spend a whole day being mindful of your posture—is your head bent forward when you drive? When you watch TV? Any prolonged period when your head is looking down is a time when you are putting excessive strain on your neck.
See Office Chair, Posture, and Driving Ergonomics
Keeping the neck straight and your phone at eye level can help prevent text neck.
Watch: Neck Strains and Sprains Video
Next, rehabilitation is important.
-
- Many people don’t know this, but you need to have strong core muscles—the abdominal and lower back muscles—to support your upper body, including your neck. Your core muscles usually do not get enough exercise during normal daily activities, so you need to do specific exercises to target these muscles.
See Core Body Strength Exercises
-
- You also need strong and flexible muscles the neck to minimize strain on your cervical spine and help support the weight of your head. Again, your neck will not get sufficient stretching and strengthening during normal daily activities, so it is best to learn specific neck exercises with the help of a health professional.
See Neck Stretches
Some people will also benefit from a more comprehensive treatment plan, such as a combination of manual adjustments, massage therapy, and cold laser therapy.
Learn more:
https://www.spine-health.com/blog/modern-spine-ailment-text-neck
Advice for headache sufferers….
Get Moving.
A new study of 573 office workers found that “one hour weekly of strength training reduced headache frequency and intensity.” Timing and spacing of session times did not affect the positive outcome, but participants whose training was supervised used fewer medications.
So, if you or someone you know suffers from headaches, call us today. Our doctors have powerful natural tools for treating headaches and can help design an exercise plan to stay healthy. Learn more about headaches here:
Source:
Andersen, CH et al. Effect of resistance training on headache symptoms in adults: Secondary analysis of a RCT. Musculoskeletal Science and Practice, Volume 32, 2017, Pages 38-43 ”
The Power Of Posture
How to use a simple posture trick to get rid of your back and neck pain!
Any posture held too long can be painful and potentially damaging; the article above is a quick way to help avoid the postural stresses that become ingrained in our daily lives now that technology has almost overcome us!

Trigger points and fibromyalgia
Myofascial pain syndrome (trigger points) and fibromyalgia are often confused to be the same condition and while there is a lot of interrelatedness between the two they are not quite identical. The clinical definition of a trigger point is “a hyper irritable spot associated within a taut band of skeletal muscle that is painful on compression or muscle contraction, and usually responds with a referred pain pattern distant from the spot”. Trigger points form from an overload trauma to the muscle tissue. This is contrasted with fibromyalgia which is defined as “a medical condition characterized by chronic widespread pain and a heightened pain response to pressure. Other symptoms include tiredness to a degree that normal activities are affected, sleep problems and troubles with memory. Some people also report restless leg syndrome, bowel and bladder problems, numbness and tingling and sensitivity to noise, lights and temperature. It is also associated with depression, anxiety, and post traumatic stress disorder”. Fibromyalgia will also present with localized tender points which are often mistaken for trigger points. Where these two conditions become somewhat interrelated is via the nervous system. Fibromyalgia patients suffer from a super-sensitization of the nervous system causing hyperirritability and pain. Myofascial trigger points can be caused by,or be the cause of, super sensitization. An active trigger point will irritate the sensory nerves around it eventually leading to super-sensitization. Trigger points have also been showed to form of become active due to super-sensitization. Both of these conditions can perpetuate the other, leading to layers of pain and symptoms. This being the case, trigger point therapy can have a very positive effect on decreasing the severity of pain and symptoms in patients suffering from fibromyalgia.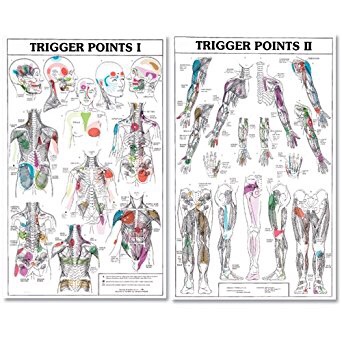

What does a shoulder separation actually mean?

The term “acromioclavicular sprain” means that you have damaged the strong fibrous bands (ligaments) that hold the end of your collarbone (clavicle) to the tip of your shoulder blade (scapula). Another term sometimes used to describe this injury is “shoulder separation.” 40-50% of all athletic shoulder injuries involve the acromioclavicular (AC) joint. AC injuries are common in adolescents and young adults who participate in contact sports, like hockey and football. Males are affected five times more often than females.
Injuries may range from mild fraying of a single ligament to complete rupture of all of the supporting ligaments. Significant tears can allow your collarbone to move upward, out of its normal position, creating a raised bump under your skin. AC joint injuries are categorized (Grade 1-Grade 6) based upon the amount of damage. Grade 1 injuries are tender without joint separation. Grade 2 injuries may be accompanied by a slight separation of the joint. Grade 3 and above will show significant joint separation.
Injuries typically occur following a fall onto the point of your shoulder, while your arm is at your side, or by falling onto your outstretched hand. You will most likely feel pain and swelling on the very top of your shoulder. More significant injuries may produce bruising or a visible “bump” beneath the skin. Moving your shoulder will likely be painfully limited for a while.
Your treatment will vary, depending upon the severity of your injury. Grade 1, 2, and most Grade 3 injuries are best managed conservatively. A sling may be used only when needed to control painful movements. Initially, you will need to limit activity, especially reaching overhead, behind your back, or across your body. The exercises described below are an important part of your rehab and should be performed consistently to avoid long-term problems. Using an ice pack for 10-15 minutes each hour may help to limit swelling and pain.
Some mild separations will heal by themselves within a week or two. More significant injuries can take longer, and disabilities typically range between one and eight weeks. Patients who have suffered a significant amount of ligament damage may have a permanent bump on their shoulder, regardless of treatment. This bump does not usually cause ongoing problems.
If you or someone you know suffers from this condition, call our office today. Our doctors are experts at relieving many types of pain including shoulder injuries.

Avoiding Back Pain At Sedentary Jobs
Some great tips on how to prevent back pain when working a sedentary job from our friends at Silicon Republic. Check out the article below.
1. Take regular breaks to stretch and walk around
Try to walk around for between three and five minutes every half hour.
2. Make sure not to hunch over while working
Everyone intuitively understands that hunching over the computer is bad for them, but it’s easy to fall into the most natural and comfortable – albeit unhealthy – sitting position while you’re in the flow of things.
3. Consider a standing desk
A standing desk offers you the opportunity to alternate your position throughout the day.



