
Don’t be afraid to look foolish.



Your spine is made up of 24 bones stacked on top of each other with a soft “disc” between each segment to allow for flexibility. Normally, each joint in your spine should move freely and independently. When one or more of your spinal vertebra is slightly misaligned and restricted, we call this condition a “spinal segmental joint restriction”. A “thoracic joint restriction” means that this misalignment or restriction is located in your upper or mid-back region.
To help visualize this, imagine a normal spine functioning like a big spring moving freely in every direction. A spine with a joint restriction is like having a section of that spring welded together. The spring may still move as a whole, but a portion of it is no longer functioning.
Joint restrictions can develop in many ways. Sometimes they are brought on by an accident or an injury. Other times, they develop from repetitive strains or poor posture. Being overweight, smoking, strenuous work, and emotional stress can make you more susceptible to problems.
Restricted joints give rise to a self-perpetuating cycle of discomfort. Joint restriction causes swelling and inflammation, which triggers muscular guarding leading to more restriction. Since your spine functions as a unit, rather than as isolated pieces, a joint restriction in one area of your spine often causes “compensatory” problems in another. Think of this as a rowboat with multiple oarsmen on each side. When one rower quits, the others are placed under additional stress and can become overworked.
Joint restrictions most commonly cause local tenderness and discomfort. You may notice that your range of motion is limited. Movement may increase your discomfort. Pain from a restricted joint often trickles around your rib cage or up & down your spine. Be sure to tell your chiropractor if your symptoms include any chest pain, shortness of breath, unusual cough, indigestion or flu- like complaints.
Long-standing restrictions are thought to result in arthritis – much like the way a slightly misaligned wheel on your car causes premature wearing of your tire.
You should recognize that your problem is common and generally treatable. Chiropractic care has been shown to be the safest and most effective treatment for joint restrictions. Our office offers several tools to help ease your pain. To speed your recovery, you should avoid activities that increase your pain. Be sure to take frequent breaks from sedentary activity. Yoga has been shown to help back pain sufferers so consider joining a class or picking up a DVD.


What is a Trigger Point?
Trigger Points (TP’s) are defined as a “hyper-irritable spot within a taut band of skeletal muscle. The spot is painful on compression and can evoke characteristic referred pain and autonomic phenomena.”1
Put into plain language, a TP is a painful knot in muscle tissue that can refer pain to other areas of the body. You have probably felt the characteristic achy pain and stiffness that TP’s produce, at some time in your life.
TP’s were first brought to the attention of the medical world by Dr. Janet G. Travell. Dr. Travell, physician to President John F. Kennedy, is the acknowledged Mother of Myofascial Trigger Points. In fact, “Trigger Point massage, the most effective modality used by massage therapists for the relief of pain, is based almost entirely on Dr. Travell’s insights.”2 Dr. Travell’s partner in her research was Dr. David G. Simons, a research scientist and aerospace physician.
Trigger Points are very common. In fact, Travell and Simons state that TP’s are responsible for, or associated with, 75% of pain complaints or conditions.1 With this kind of prevalence, it’s no wonder that TP’s are often referred to as the “scourge of mankind”.
Trigger Points can produce a wide variety of pain complaints. Some of the most common are migraine headaches, back pain, and pain and tingling into the extremities. They are usually responsible for most cases of achy deep pain that is hard to localize.
A TP will refer pain in a predictable pattern, based on its location in a given muscle. Also, since these spots are bundles of contracted muscle fibres, they can cause stiffness and a decreased range of motion. Chronic conditions with many TP’s can also cause general fatigue and malaise, as well as muscle weakness.
Trigger Points are remarkably easy to get, but the most common causes are
TP’s (black X) can refer pain to other areas (red)
Sudden overload of a muscle
Once in place, a TP can remain there for the remainder of your life unless an intervention takes place.
Trigger Points Not Well Known
With thousands of people dealing with chronic pain, and with TP’s being responsible for — or associated with — a high percentage of chronic pain, it is very disappointing to find that a large portion of doctors and other health care practitioners don’t know about TP’s and their symptoms.
Scientific research on TP’s dates back to the 1700’s. There are numerous medical texts and papers written on the subject.
But, it still has been largely overlooked by the health care field. This has led to needless frustration and suffering, as well as thousands of lost work hours and a poorer quality of life.
How Are Trigger Points Treated?
As nasty and troublesome as TP’s are, the treatment for them is surely straight-forward. A skilled practitioner will assess the individual’s pain complaint to determine the most likely location of the TP’s and then apply one of several therapeutic modalities, the most effective of which is a massage technique called “ischemic compression”.
Basically, the therapist will apply a firm, steady pressure to the TP, strong enough to reproduce the symptoms. The pressure will remain until the tissue softens and then the pressure will increase appropriately until the next barrier is felt. This pressure is continued until the referral pain has subsided and the TP is released. (Note: a full release of TP’s could take several sessions.)
Other effective modalities include dry needling (needle placed into the belly of the TP) or wet needling (injection into the TP). The use of moist heat and stretching prove effective, as well. The best practitioners for TP release are Massage Therapists, Physiotherapists, and Athletic Therapists. An educated individual can also apply ischemic compression to themselves, but should start out seeing one of the above therapists to become familiar with the modality and how to apply pressure safely.
1 Simons, D.G., Travell, D.G., & Simons, L.S. Travell and Simons’Myofascial Pain and Dysfunction: the Trigger Point Manual.
Vol. 1. 2nd ed. Lippincott, Williams, and Wilkins, 1999.

The muscles of the hip provide not only local stability, but also play an important role in spinal and lower extremity functional alignment. (1-4) While weakness in some hip muscles (hip extensors and knee extensors) is well tolerated, weakness or imbalance in others can have a profound effect on gait and biomechanical function throughout the lower half of the body. (5) Weakness of the hip abductors, particularly those that assist with external rotation, has the most significant impact on hip and lower extremity stability. (5,6)
The gluteus medius is the principal hip abductor. When the hip is flexed, the muscle also assists the six deep hip external rotators (piriformis, gemelli, obturators, and quadratus femoris). The gluteus medius originates on the ilium just inferior to the iliac crest and inserts on the lateral and superior aspects of the greater trochanter. While the principal declared action of the gluteus medius is hip abduction, clinicians will appreciate its more valuable contribution as a dynamic stabilizer of the hip and pelvis- particularly during single leg stance activities like walking, running, and squatting. The gluteus medius contributes approximately 70% of the abduction force required to maintain pelvic leveling during single leg stance. The remainder comes predominantly from 2 muscles that insert onto the iliotibial band: the tensor fascia lata and upper gluteus maximus. Hip abductor strength is the single greatest contributor to lower extremity frontal plain alignment during activity. (6)
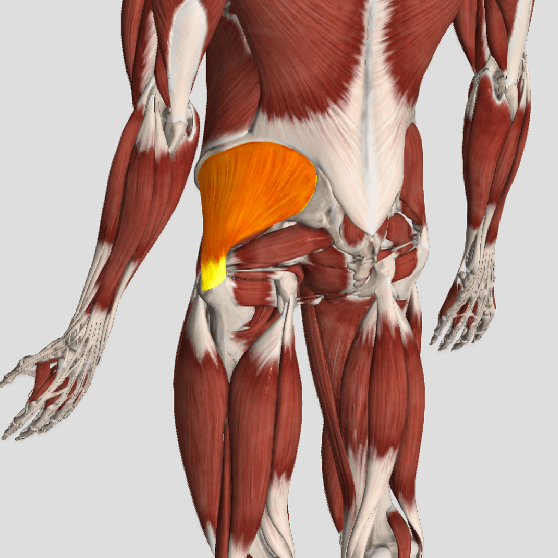
Incompetent hip abductors and/or external rotators allows for excessive adduction and internal rotation of the thigh during single leg stance activities. This leads to a cascade of biomechanical problems, including pelvic drop, excessive hip adduction, excessive femoral internal rotation, valgus knee stress, and internal tibial rotation. (1,7-12)

Patellofemoral pain syndrome (PFPS), also called “Runners Knee”, describes the symptom complex of knee discomfort, swelling, or crepitus that results from excessive or imbalanced forces acting on the joint. It is the most common cause of knee pain in the general population, affecting an estimated 25% of adults.
PFPS is most commonly related to lateral tracking of the patella. The patella has a natural tendency to migrate laterally due to the pull of the quadriceps and the slight natural valgus of the lower extremity. A new study in the Journal of Sports Medicine (1) provides additional confirmation that when managing patellofemoral pain syndrome, clinicians must address two critical yet often overlooked issues.
This study concludes that PFPS and dynamic knee valgus do not arise primarily from knee dysfunction, rather from hip abductor/ external rotator weakness and/or foot hyperpronation.
“The most effective intervention programs included exercises targeting the hip external rotator and abductor muscles and knee extensor muscles.” and “PFPS patients with foot abnormalities, such as those with increased rearfoot eversion or pes pronatus, may benefit the most from foot orthotics.”
Since gluteus medius and VMO weakness are key factors in the development of PFPS, strengthening exercises that target those muscles prove most effective. Stabilization exercises may include pillow push (push the back of your knee into a pillow for 5-6 seconds), supine heel slide, terminal knee (short-arc) extension, clam, glut bridge, semi-stiff deadlift, posterior lunge, and monster walk.
Myofascial release and stretching should be directed at hypertonic muscles, including the TFL, gastroc, soleus, hamstring, piriformis, hip rotators, and psoas. Myofascial release or IASTM may be appropriate for tightness in the iliotibial band, vastus lateralis, posterior hip capsule, and lateral knee retinaculum.
Manipulation may be necessary for restrictions in the lumbosacral and lower extremity joints. Hypermobility is common in the ipsilateral SI joint with restrictions present contralaterally. Evidence has shown that patellar tracking braces, i.e. BioSkin® or PatellaPro®, may lead to better outcomes.
Lifestyle modification may be necessary to reduce pain-provoking endeavors, especially running, jumping and other activities that induce a valgus stress. Athletes should avoid allowing their knee to cross in front of their toes while squatting. Arch supports or custom orthotics may be necessary to correct hyperpronation. Runners should avoid cross-over gaits and change shoes every 250 to 500 miles.
.
.
.
.
.
.
.
#pain
#kneepain
#chiropractic
#fitness
#sports
#wellness
#fitness
#healthyliving
#healthychoices
#Winnipeg
References
1. Petersen W, Rembitzki I, Liebau C. Patellofemoral pain in athletes. Open Access Journal of Sports Medicine. 2017;8:143-15

Becoming healthy and staying healthy is hard, challenging work but worth every second of persistence.

Moving is good for your back and muscles, especially if you have back pain.

In today’s fast-paced world, stress has become an inevitable part of daily life for many people. From demanding work schedules to personal responsibilities, the pressures of modern living can take a toll on our physical, mental, and emotional well-being. While there are numerous strategies for managing stress, one alternative therapy that has gained attention for its potential effectiveness is acupuncture. But does acupuncture really help relieve stress, or is it just a myth? In this article, we’ll explore the science behind acupuncture for stress relief and examine the evidence supporting its use as a therapeutic tool.
Understanding Acupuncture
Acupuncture is an ancient healing practice that originated in China thousands of years ago. It involves the insertion of thin needles into specific points on the body known as acupuncture points or acupoints. According to traditional Chinese medicine (TCM) theory, the human body contains meridians or energy pathways through which vital energy, known as Qi (pronounced “chee”), flows. By stimulating acupoints along these meridians, acupuncturists aim to restore the balance and flow of Qi, thereby promoting health and well-being.
The Stress Response and Acupuncture
Stress is the body’s natural response to perceived threats or challenges, triggering a cascade of physiological and psychological reactions designed to help us cope with or escape from danger. While short-term stress can be beneficial, chronic or excessive stress can have detrimental effects on our health, contributing to a wide range of physical and mental health problems, including anxiety, depression, insomnia, digestive issues, and cardiovascular disease.
Research suggests that acupuncture may help modulate the body’s stress response and promote relaxation through various mechanisms:
Scientific Evidence Supporting Acupuncture for Stress Relief
While more research is needed to fully understand the mechanisms underlying acupuncture’s effects on stress, numerous studies have demonstrated its potential efficacy in reducing stress levels and improving stress-related symptoms. For example:
Conclusion
While acupuncture may not be a cure-all for stress, the growing body of research suggests that it can be a valuable tool for stress management and relaxation. By modulating neurotransmitter activity, balancing hormonal levels, regulating the autonomic nervous system, and reducing muscle tension, acupuncture offers a holistic approach to stress relief that addresses both the physical and psychological aspects of stress. If you’re struggling with stress or looking for natural ways to promote relaxation and well-being, consider exploring acupuncture as part of your self-care routine.