Whiplash is an injury to the soft-tissues of the neck often referred to as a sprain or strain. Because there are a unique set of symptoms associated with whiplash, doctors and researchers commonly use the term “whiplash associated disorders” or WAD to describe the condition.
WAD commonly occurs as a result of a car crash, but it can also result from a slip and fall, sports injury, a personal injury (such as an assault), and other traumatic causes. The tissues commonly involved include muscle tendons (“strain”), ligaments and joint capsules (“sprains”), disk injuries (tears, herniation), as well as brain injury or concussion—even without hitting the head!
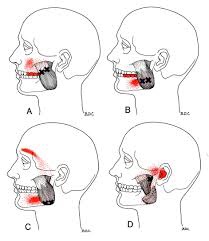
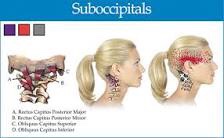
Symptoms vary widely but often include neck pain, stiffness, tender muscles and connective tissue (myofascial pain), headache, dizziness, sensations such as burning, prickly, tingling, numbness, muscle weakness, and referred pain to the shoulder blade, mid-back, arm, head, or face. If concussion occurs, additional symptoms include cognitive problems, concentration loss, poor memory, anxiety/depression, nervousness/irritability, sleep disturbance, fatigue, and more!
Whiplash associated disorders can be broken down into three categories: WAD I includes symptoms without any significant examination findings; WAD II includes loss of cervical range of motion and evidence of soft-tissue damage; and WAD III includes WAD II elements with neurological loss—altered motor and/or sensory functions. There is a WAD IV which includes fracture, but this is less common and often excluded.
Treatment for WAD includes everything from doing nothing to intensive management from multiple disciplines—chiropractic, primary care, physical therapy, clinical psychology, pain management, and specialty services such as neurology, orthopedics, and more. The goal of treatment is to restore normal function and activity participation, as well as symptom management.
The prognosis of WAD is generally good as many will recover without residual problems within days to weeks, with most people recovering around three months after the injury. Unfortunately, some are not so lucky and have continued neck pain, stiffness, headache, and some develop post-concussive syndrome. The latter can affect cognition, memory, vision, and other brain functions. Generally speaking, the higher the WAD category, the worse the prognosis, although each case MUST be managed by its own unique characteristics. If the injury includes neurological loss (muscle strength and/or sensory dysfunction like numbness, tingling, burning, pressure), the prognosis is often worse.
Chiropractic care for the WAD patient can include manipulation, mobilization, and home-based exercises, as well as the use of anti-inflammatory herbs (ginger, turmeric, proteolysis enzymes (bromelain, papain), devil’s claw, boswellia extract, rutin, bioflavonoid, vitamin D, coenzyme Q10, etc.) and dietary modifications aimed at reducing inflammation and promoting healing.
* 83% of those patients involved in an MVA will suffer whiplash injury and 50% will be symptomatic at 1 year.
* 90% of patients with neurologic signs at onset may be symptomatic at 1 year.
* 25- 80% of patients who suffer a whiplash injury will experience late-onset dizziness
* Clinicians should be observant for radiographic signs of instability, including interspinous widening, vertebral subluxation, vertebral compression fracture, and loss of cervical lordosis.
* Horizontal displacement of greater than 3.5 mm or angular displacement of more than 11 degrees on flexion/extension views suggests instability.