These muscles are located in the groin. The longus originates on the pubic body just below the pubic crest and inserts on the middle third of the linea aspera.The brevis muscle originates on the inferior ramus and body of the pubis and has its attachment to the lesser trochanter and linea aspera of the femur. Trigger points in these muscles are the most common muscular cause of groin pain. Distal trigger points refer pain to the upper medial knee and down the tibia. Proximal trigger points refer into the anterior hip area.
Sleep
Trigger points in the temporalis muscle
The temporalis muscle is located in the temple area of the skull. It originates on the temporal lines on the parietal bone of the skull, and inserts on the coronoid process of the mandible. It’s main action is to close the jaw. The posterior and middle fibres bilaterally retrude the mandible. Acting individually, this muscle will deviate the mandible to the same side. Trigger points in this muscle refer into the teeth causing hypersensitivity, and into and above the eye and temple, causing headaches.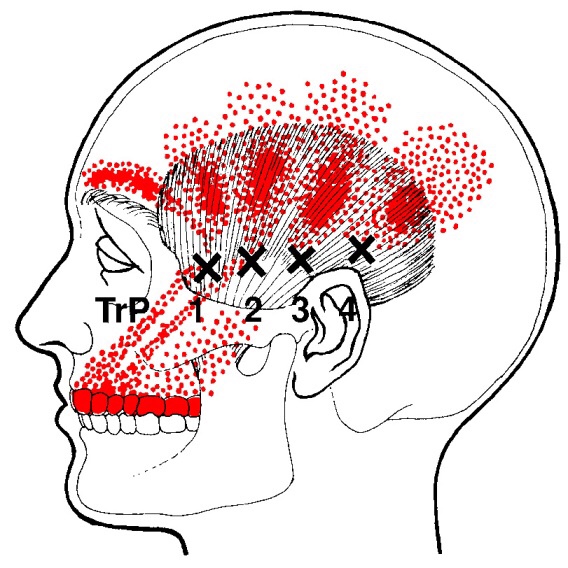
What is a “Mild” traumatic Brain Injury?
A concussion is a blow or jolt to the head that disrupts normal brain function. Concussions, also known as Mild Traumatic Brain Injuries, most often result from falls, sports injuries, and auto accidents.
 Concussion symptoms may begin immediately after an injury, but sometimes take hours or days to appear. The most common symptoms of a concussion include; headaches, light-headedness, dizziness, visual disturbances, ringing in the ears, confusion, fatigue, difficulty sleeping, irritability, and difficulty remembering or learning new things. Patients sometimes struggle to understand conversations or make simple calculations like determining a restaurant tip. Patients often feel as if they are “in a fog”. Symptoms can range from subtle to debilitating.
Concussion symptoms may begin immediately after an injury, but sometimes take hours or days to appear. The most common symptoms of a concussion include; headaches, light-headedness, dizziness, visual disturbances, ringing in the ears, confusion, fatigue, difficulty sleeping, irritability, and difficulty remembering or learning new things. Patients sometimes struggle to understand conversations or make simple calculations like determining a restaurant tip. Patients often feel as if they are “in a fog”. Symptoms can range from subtle to debilitating.
Patients and their attendants should be particularly alert for signs or symptoms that could indicate a more threatening injury like; worsening headache, growing irritability, repeated vomiting, difficulty speaking or swallowing, shortness of breath, unequal pupils, fever, visual disturbances, seizures, clear discharge from the nose or ears, loss of consciousness, or increasing light-headedness, numbness, or confusion. These symptoms warrant immediate emergency medical attention.
Recovery times are quite variable and are dependent upon a number of factors. It is critical that you allow your brain to recover completely before returning to physical activity. A concussion can be likened to dropping a computer – you will need to allow time to reboot before trying to use it. Suffering a second concussion before the first has completely resolved can lead to significantly worse symptoms and long-term impairments.
Athletes who have suffered a concussion must not return to activity before being evaluated by a healthcare professional that is very familiar with concussion management.
Meditation goes mainstream!
With growing evidence that meditation has significant health benefits, a 2016 study by a team of researchers from the United States, Spain, and France sought to explain how and why meditation actually works.
The study investigated the difference between “mindful meditation” in a group of experienced meditators vs. “quiet non-meditative activity” in a group of untrained control subjects. After eight hours of mindfulness practice, the meditation group showed a range of genetic and molecular differences, which in turn correlated with faster physical recovery from a stressful situation.
According to researchers, this is the first time a study has documented a rapid alteration in gene expression within meditating subjects. Interestingly, the researchers observed these changes in the SAME genes that anti-inflammatory and pain-killing drugs target! Thus, they speculate that mindful-based training may benefit patients with inflammatory conditions! This and prior studies have prompted the American Heart Association to endorse meditation as an effective cardiac preventative intervention.
Meditation has been found to be helpful for many conditions including stress management, lowering high blood pressure, heart disease, and depression. You can incorporate meditation into your life with three simple meditation exercises! The initial advice is “…go slow and be compassionate and gentle with yourself.” Your mind will try to wander (called our “default mode”) which consumes about half of our day, so try to focus (called “focus mode”)!
1) WALKING MEDITATION: At a slow to medium pace, focus on your feet. Notice how your heel hits the ground and then feel the roll of your foot followed by the big toe pushing off prior to the swing phase. Feel for stones under the foot and other interesting sensations. If your mind starts to wander (default mode), gently bring your attention back to your foot (focus mode). You WILL get better with practice, and you’ll soon find it much easier to “focus” during stressful situations!
2) NOVEL EXPERIENCES: It’s much easier to lose focus on the people you see everyday vs. those seen only one time a month. The next time you arrive home from work, pretend you haven’t seen your spouse/friend in 30 days. Give them your undivided attention. Then, try this on co-workers and other people you see every day. Believe me, they WILL notice a difference!
3) GRATITUDE EXERCISES: When you’re not in their presence, focus on a person’s face and send them a “silent gratitude” for being in your life. Try this on family members, friends, co-workers, and others!
Trigger points in the triceps muscle.
The tricep muscle is named for its three heads long, medial, and lateral. The long head originates on the infraglenoid tubercle, the medial head on the posterior humerus, and the lateral head on the posterior humerus as well. They join together to insert on the Olecranon process of the ulna. The triceps function to extend the elbow. Strong extension under resistance can cause trigger points to form. Pain referred from triceps trigger points can be felt in the posterior shoulder and down the posterior forearm, as well as in in the olecranon process and the lateral epicondyle which can cause “tennis elbow” pain.
Some Sleep Habit Tips

Researchers recommend sleeping for 7-9 hours per night. Even small deficits can pose problems like decreased athleticism, diminished brain function, increased inflammation and a greater likelihood to get sick- sleeping only 6 hours per night makes you four times more likely to catch a cold when compared to sleeping 7 or more hours. Follow these additional tips for better sleep:
✓ Limit screen time before retiring- the blue light emitted from computer monitors, phones and TV’s can limit melatonin production and adversely affect sleep. Try reading from a book or magazine instead.
✓ Ideally, eat your last meal 3-4 hours before bedtime and especially limit heavy, spicy or high-fat foods. Ration how much you drink before bedtime to minimize bathroom breaks. Particularly limit caffeine in the afternoon and evening- caffeine has a half-life of 6-9 hours and can keep you awake long after the last sip.
✓ Stick to a sleep schedule, trying to retire and arise at the same time each day, including weekends.
✓ Sleep on a comfortable mattress and pillow. Choose 100% cotton sleep clothes and sheets over synthetic materials (i.e. polyester). Some research has suggested that your “deep” REM sleep improves when your mattress is oriented so that your body is aligned North and South as opposed to East and West.
✓ Most people sleep best in a cool room; ideally between 60-67 degrees F.
Pathophysiology of trigger points.
A large number of factors have been identified as causes of trigger point activation. These include acute or chronic overload of muscle tissue, disease, psychological distress, systemic inflammation, homeostatic imbalances, direct trauma, radiculopathy, infections, and lifestyle choices such as smoking. Trigger points form as a local contraction of muscle fibres in a muscle or bundle of muscle fibres. These can pull on ligaments and tendons associated with the muscle which can cause pain to be felt deep inside a joint. It is theorized that trigger points form from excessive release of acetylcholine causing sustained depolarization of muscle fibres. Trigger points present an abnormal biochemical composition with elevated levels of acetylcholine, noradrenaline and serotonin and a lower ph. The contracted fibres in a trigger point constricts blood supply to the area creating an energy crisis in the tissue that results in the production of sensitizing substances that interact with pain receptors producing pain. When trigger points are present in a muscle there is often pain and weakness in the associated structures. These pain patterns follow specific nerve pathways that have been well mapped to allow for accurate diagnosis or the causative pain factor.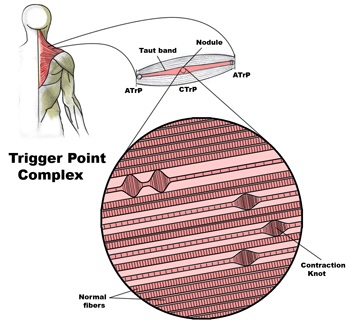
What is a trigger point
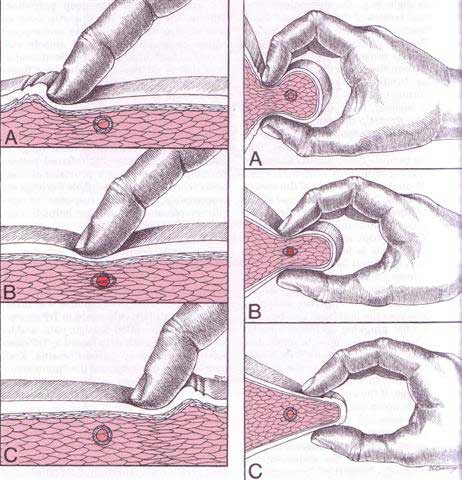
Dr Janet travel coined the term trigger point in 1942 to describe clinical findings with characteristics of pain related a discrete irritable point in muscle or fascia that was not caused by acute trauma, inflammation, degeneration, neoplasm or infection. The painful point can be palpated as a nodule or tight band in the muscle that can produce a local twitch response when stimulated. Palpation of the trigger point reproduces the pain and symptoms of the patient and the pain radiates in a predictable referral pattern specific to the muscle harbouring the trigger point.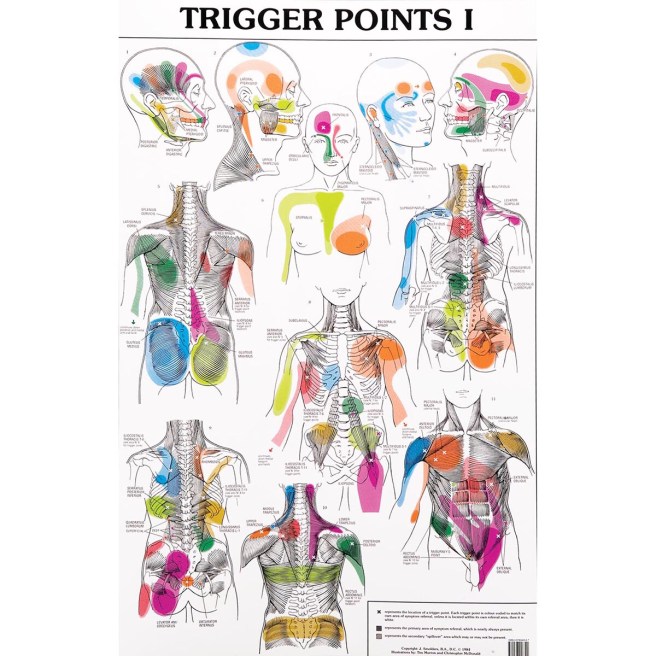
What to expect with a trigger point massage.
A treatment with Bryan is very user friendly. And, no, you don’t have to remove any clothing. However, bringing a t-shirt and a pair of shorts or sweats is recommended.
The first time you come for a treatment you will be asked to fill out a Client History form. Bryan will go over the information you provide, asking for more detail and discussing the type of pain you are having and its location.
The treatment itself involves locating the Trigger Points in the muscle or soft tissue and applying a deep focused pressure to the Point. This will reproduce the pain and the referral pattern that is characteristic of that pain.
The treatment will be uncomfortable at first, but as the Trigger Points release, the pain will decrease. The pressure will always be adjusted to your tolerance level. If, at any time, you feel too uncomfortable you can ask Bryan to ease off a bit.
Depending on your specific problem, Bryan may also use some stretching and / or range-of-motion techniques, as needed.
After treatment, it is usually recommended that the client apply moist heat to the area treated.
CTS at Night.
For those who have carpal tunnel syndrome (CTS), it’s no surprise that CTS is frequently most expressive during the night, often to the point of interrupting sleep and/or making it difficult to fall back to sleep. So why is that?
The primary reason for nighttime CTS symptoms has to do with the wrist, as it is very difficult to sleep with the wrist held in its “ideal” or least irritating position. In fact, most people favor “curling” the back of the hand under the chin or bending the hand/wrist backwards under the head. When the wrist is bent in either direction, it can increase the pressure inside the wrist, which can generate the various symptoms associated with CTS.
One study evaluated the pressure inside the carpal tunnel while participants slowly moved their wrists. The researchers found many movements didn’t need to exceed 20 degrees before the pressure increased enough within the carpal tunnel to generate symptoms.
Because it doesn’t take a lot of movement to build up excessive pressure in the wrists of those with CTS, many doctors recommend the use of a “cock-up splint” for the non-surgical treatment of CTS in order to help keep the wrist in a neutral position.
Wrist posture is also an important factor during the day. One study looked at typing on a tablet PC, which allowed people to work in non-traditional settings. As screen size reduced, the posture required to type became more limited and accelerated the usual rate of pain onset in the neck, elbows, and wrists.
This study also looked at three different positions used when working on touch-screen devices: desk, lap, and bed. The healthy subjects completed six, 60-minute typing sessions using three virtual keyboard designs: standard, wide, and split. The researchers monitored the position of the wrist, elbow, and neck while the participants typed and followed up each session with questionnaires designed to measure discomfort.
The research team reported that typing in bed required greater wrist extension but resulted in a more natural elbow position than typing at a desk. The angled split keyboard significantly reduced the wrist deviation vs. the standard or wide keyboard designs. All three regions—the neck, elbow, and wrist—exhibited more movements (13% to 38%) towards the end of the one hour sessions, which correlated with a significant increase in pain in every body region investigated. Overall, using a wider keyboard while sitting at a desk was the most tolerable position among study participants.


