Temporomandibular joint dysfunction is a blanket term that refers to pain and dysfunction of the jaw muscles and the tempomandibular joints which connect the mandible to the skull. The most common symptoms are pain and restricted mandibular movement as well as grinding noises coming from the joint. This condition is more common in women then in men, and affects a large portion of patients suffering from fibromyalgia. Trigger points in the muscles of mastication are frequently involved in TMJ dysfunction. Trigger points in the pterygoid and masseter muscles for example will not only refer pain into the tempomandibular joints, but will also cause a dysfunctional movement pattern that can restrict range of motion. Trigger point therapy can be an effective modality to treat TMJ dysfunction.

Posture
I smoke and I sit; does that matter?
Your thoracic spine is made up of 12 individual vertebrae stacked on top of each other. To allow for flexibility and movement, there is a cushion or “disc” in between each level. As we age, these discs can wear and become thinner over time. This leads to additional changes, including bone spurs and narrowing of the opening where your nerves exit your spine. This process is called “thoracic spondylosis”, or simply, “arthritis”.

How quickly you develop back arthritis is largely a trait you inherited from your parents. Other factors may play a role, including a history of trauma, smoking, operating motorized vehicles, being overweight and/ or performing repetitive movements (i.e. lifting, twisting, bending or sitting). Men seem to be affected slightly more often than women.
Symptoms often begin as back pain that gradually worsens over time. Stiffness may be present upon arising in the morning. Pain is relieved by rest or light activity and aggravated by strenuous work. Sometimes your nerves can become “pinched” in narrowed openings where they exit your spine. This can cause pain, numbness, or tingling radiating around your trunk along the path of the irritated nerve. Be sure to tell your doctor if you notice any weakness or if you have a rash (running along your rib), fever, abdominal pain, change in bowel or bladder function, or pain in your groin crease.
Arthritic changes can be seen on x-rays, but interestingly, the amount of wearing does not seem to correlate directly with the severity of your symptoms. People with the same degree of arthritis may have symptoms ranging from none to severe. Most researchers believe that the symptoms of osteoarthritis are not the direct result of the disease, but rather, from the conditions that preceded the disease and those that develop after it, like joint restrictions and muscle tightness. Fortunately, those conditions are treatable and our office has a variety of tools to help relieve your pain.
In general, you should avoid repeated lifting and twisting and take frequent breaks from prolonged sitting, especially in motorized vehicles. Avoid any position that causes an increase in radiating pain. Light exercise, like walking, stationary cycling, water aerobics, and yoga may be helpful. Smokers should find a program to help them quit and overweight patients will benefit from a diet and exercise program.
Trigger points and fibromyalgia
Myofascial pain syndrome (trigger points) and fibromyalgia are often confused to be the same condition and while there is a lot of interrelatedness between the two they are not quite identical. The clinical definition of a trigger point is “a hyper irritable spot associated within a taut band of skeletal muscle that is painful on compression or muscle contraction, and usually responds with a referred pain pattern distant from the spot”. Trigger points form from an overload trauma to the muscle tissue. This is contrasted with fibromyalgia which is defined as “a medical condition characterized by chronic widespread pain and a heightened pain response to pressure. Other symptoms include tiredness to a degree that normal activities are affected, sleep problems and troubles with memory. Some people also report restless leg syndrome, bowel and bladder problems, numbness and tingling and sensitivity to noise, lights and temperature. It is also associated with depression, anxiety, and post traumatic stress disorder”. Fibromyalgia will also present with localized tender points which are often mistaken for trigger points. Where these two conditions become somewhat interrelated is via the nervous system. Fibromyalgia patients suffer from a super-sensitization of the nervous system causing hyperirritability and pain. Myofascial trigger points can be caused by,or be the cause of, super sensitization. An active trigger point will irritate the sensory nerves around it eventually leading to super-sensitization. Trigger points have also been showed to form of become active due to super-sensitization. Both of these conditions can perpetuate the other, leading to layers of pain and symptoms. This being the case, trigger point therapy can have a very positive effect on decreasing the severity of pain and symptoms in patients suffering from fibromyalgia.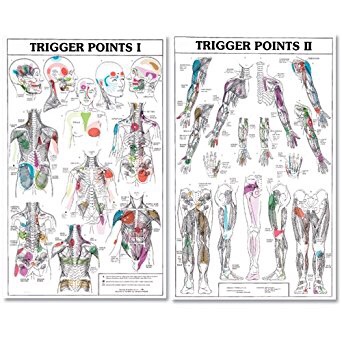

Mobility Myth #1
Great stuff from our friends at Shape.com:
Myth: Stretching and foam rolling will address all of my mobility problems.
Truth: Stretching and soft tissue work (like foam rolling and massage) may seem like the bread and butter of mobility, but there’s more to know. “If you have a true mechanical mobility problem, soft tissue work and different stretching techniques are definitely great options,” says Ardoin. But you might experience tightness or a loss of motion that doesn’t have anything to do with tissue restrictions like tight muscles or joint stiffness.
“In these particular people, they actually have the mobility needed, but their brain doesn’t know how to access it,” says Ardoin. This sort of muscle-brain disconnect could be because of current pain, previous injuries, or, “sometimes people just forget how to move,” he says.
In this case, your muscles are working against each other instead of synergistically—and it’s not something stretching or foam rolling will fix. The good news is that there’s not actually anything physically wrong. The bad news: This is tough to diagnose on your own. “If you have a loss of motion while you perform the motion yourself but have full ROM when performed passively, then it’s safe to assume that you have the ROM available but your brain doesn’t know how to access it,” says Ardoin.
For example, let’s say you have a “tight” shoulder. Make a large, slow circle with your right arm. Then totally relax your arm while someone else rotates your arm in a circle for you. Did it go farther while you let the motion happen passively? Ding, ding! Could be a brain problem, not a muscle problem. Think this might be you? Seeing a trainer or physical therapist to confirm it (and help you work on the issue) can’t hurt.
The Thoracic Disc Lesion
Your spine consists of 24 individual vertebrae stacked on top of each other. Flexible cushions called “discs” live between each set of vertebra. A disc is made up of two basic parts. The inner disc, called the “nucleus” is like a ball of jelly about the size of a marble. This jelly is held in place by the outer part of the disc called the “annulus,” which is wrapped around the inner nucleus,

much like a ribbon wrapping around your finger. The term “thoracic disc lesion” means that one or more of the 12 discs in the center section of your spine has been damaged.
Disc problems start when the outer fibers of the disc become strained or frayed. If enough fibers become frayed, the disc weakens and when compressed, may “bulge” like a weak spot on an inner tube. If more fibers are damaged, the nucleus of the disc may “herniate” out of the disc.
Surprisingly, thoracic disc bulges are present without any symptoms in almost half of the adult population. Disc bulges that cause pain commonly occur in the neck or lower back but are relatively infrequent in the thoracic spine – accounting for less than 1% of all symptomatic disc problems. The condition is most common between the ages of 40 and 60. Certain occupations or activities place you at greater risk, especially physically demanding activities that involve repetitive twisting, awkward postures.
Pain can range from dull, localized discomfort to sharp, radiating pain. Your symptoms may change unpredictably. If the disc bulge is bad enough to compress your nerve, you could experience sharp, burning, or shooting pain in a band-like distribution around your rib cage. Thoracic disc herniations commonly mimick other conditions like heart or lung problems. Be sure to let our office know if you notice chest pressure; shortness of breath; pain radiating into your arm, face, or jaw; pain with deep breathing; clumsiness; loss of bowel or bladder control; unexplained weight loss; night sweats; pain that awakens you at night; fever; indigestion; nausea; flu-like symptoms or if you notice a rash following the margin of one of your ribs.
You should avoid excessive bed rest while recovering. Researchers have shown that disc bulges may be successfully managed with exercise and conservative care, like the type we will provide.
Trigger points in the adductor longus and brevis.
These muscles are located in the groin. The longus originates on the pubic body just below the pubic crest and inserts on the middle third of the linea aspera.The brevis muscle originates on the inferior ramus and body of the pubis and has its attachment to the lesser trochanter and linea aspera of the femur. Trigger points in these muscles are the most common muscular cause of groin pain. Distal trigger points refer pain to the upper medial knee and down the tibia. Proximal trigger points refer into the anterior hip area.
“I Popped A Rib”
You have 12 pair of ribs that attach to the “thoracic” region of your spine. The ribs serve to protect your heart, lungs, and other vital organs. Each rib is shaped much like a “bucket handle” arching from your spine to your breastbone (sternum) in front. Your ribs must move freely when you breathe, bend, twist, and reach. The term “costovertebral dysfunction” means that one or more of your ribs has become restricted or slightly malpositioned from it’s attachment to the spine.
 You can visualize this as imagining one of your bucket handles is misaligned and not moving in sync with the others.
You can visualize this as imagining one of your bucket handles is misaligned and not moving in sync with the others.
Rib problems can develop in many ways. Sometimes they are brought on by an accident or injury; other times, they develop from repetitive strains or poor posture. Rib malpositions are common during pregnancy or after a whiplash injury.
Symptoms sometimes begin following a sudden or explosive movement, like coughing or sneezing, reaching, pushing, or pulling. Other times, a specific cause cannot be recalled. Rib dysfunction may cause pain near or slightly to the side of your spine with possible radiation of symptoms along your rib, sometimes all the way to the front. Some patients feel as though they were “shot by an arrow.” Rib problems are a frequently overlooked source of chest and abdominal pain.
Be sure to tell your chiropractor if your symptoms include any unusual cough, indigestion, nausea, vomiting, fever, flu-like complaints or if you notice a rash developing along the border of your rib. Seek immediate medical treatment if you notice chest “pressure” or “squeezing”, symptoms that radiate into your arm and jaw, or if you have chest pain or shortness of breath with exertion, as these are possible symptoms of heart problems and must be addressed immediately.
Most patients report rapid relief following chiropractic care. Our office can provide several tools to help ease your pain. To speed your recovery, you should avoid activities that increase your pain. Initially, you may need to limit reaching, pushing, and pulling. Women may benefit by temporarily switching to a sports bra to help better diffuse pressure over irritated ribs. Some patients report relief by using sports creams, NSAIDs, or applying ice for 15-20 minutes directly over the painful area.
Avoiding Back Pain At Sedentary Jobs
Some great tips on how to prevent back pain when working a sedentary job from our friends at Silicon Republic. Check out the article below.
1. Take regular breaks to stretch and walk around
Try to walk around for between three and five minutes every half hour.
2. Make sure not to hunch over while working
Everyone intuitively understands that hunching over the computer is bad for them, but it’s easy to fall into the most natural and comfortable – albeit unhealthy – sitting position while you’re in the flow of things.
3. Consider a standing desk
A standing desk offers you the opportunity to alternate your position throughout the day.
Right between my shoulder blades, Doc…..
Your spine is made up of 24 bones stacked on top of each other with a soft “disc” between each segment to allow for flexibility. Normally, each joint in your spine should move freely and independently. Our examination of your spine has shown that one or more of your spinal vertebra is slightly misaligned and restricted. We call this condition “spinal segmental joint restriction”.

To help visualize this, imagine a normal spine functioning like a big spring moving freely in every direction. A spine with a joint restriction is like having a section of that spring welded together. The spring may still move as a whole, but a portion of it is no longer functioning.
Joint restrictions can develop in many ways. Sometimes they are brought on by an accident or an injury. Other times, they develop from repetitive strains or poor posture. Being overweight, smoking, strenuous work, and emotional stress can make you more susceptible to problems.
Restricted joints give rise to a self-perpetuating cycle of discomfort. Joint restriction causes swelling and inflammation, which triggers muscular guarding leading to more restriction. Since your spine functions as a unit, rather than as isolated pieces, a joint restriction in one area of your spine often causes “compensatory” problems in another. Think of this as a rowboat with multiple oarsmen on each side. When one rower quits, the others are placed under additional stress and can become overworked.
Joint restrictions most commonly cause local tenderness and discomfort. You may notice that your range of motion is limited. Movement may increase your discomfort. Pain from a restricted joint often trickles around your rib cage or up & down your spine. Be sure to tell your chiropractor if your symptoms include any chest pain, shortness of breath, unusual cough, indigestion or flu-like complaints.
Long-standing restrictions are thought to result in arthritis – much like the way a slightly misaligned wheel on your car causes premature wearing of your tire.
You should recognize that your problem is common and generally treatable. Chiropractic care has been shown to be the safest and most effective treatment for joint restrictions. Our office offers several tools to help ease your pain. To speed your recovery, you should avoid activities that increase your pain. Be sure to take frequent breaks from sedentary activity. Yoga has been shown to help back pain sufferers so consider joining a class or picking up a DVD.
Trigger points in the Quadratus Lumborum muscle.
The quadratus lumborum muscle is a commonly overlooked source of low back pain and is often responsible for “pseudo disc syndrome”. This muscle originates on the inferior border of the 12th rib and lumbar transverse processes. It inserts on the iliac crest and iliolumbar ligament. The q.l.’s main actions are extension and lateral flexion of the spine. It also acts as a stabilizer of the lumbar spine. Trigger points in this muscle refer pain into the sacroiliac joint and the lower buttock. Pain can also spread anteriorly along the crest of the ilium into the lower abdomen and groin and to the greater trochanter. 

