Cervical spondylosis (CS) is another term for osteoarthritis (OA) of the neck. It is a common, age-related condition that you will probably develop if you live long enough. Or, if you suffered a neck injury as a youth, it can develop within five to ten years of the injury, depending on the severity. According to the Mayo Clinic, CS or OA affects more than 85% of people over 60 years old, and that is probably a conservative estimate!
Common symptoms associated with CS/OA vary widely from no symptoms whatsoever to debilitating pain and stiffness. For example, when CS crowds the holes through which the nerves and/or spinal cord travel, it creates a condition called spinal stenosis that can result in numbness, tingling, and/or weakness. In severe cases, this can even affect bowel or bladder control (which is an EMERGENCY)!
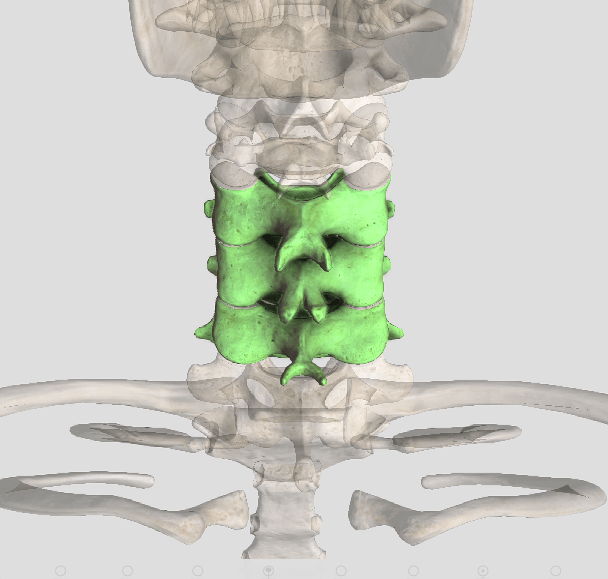
CS occurs when the normal slippery, shiny cartilage surfaces of the joint(s) gradually thin and eventually wear away. Bone spurs often form, which results from the body trying to stabilize an unstable joint. In some cases, the spurs can actually fuse a joint, which often helps reduce pain. (Bone spurs can also form if the intervertebral disks or shock-absorbing pads between the vertebrae are injured or become dehydrated due to arthritic conditions.)
Risk factors associated with CS include: aging, injury, years of heavy lift/carry job demands, and jobs and/or hobbies that require the neck to be outside of a neutral position (like years of pinching a phone between the ear and shoulder). Genetics and bad habits (like smoking) also play a role in CS. Obesity and inactivity also worsens the severity of CS symptoms.
The good news is that even though most of us will have CS, it is usually NOT a disabling condition. However, CS may interfere with our normal activities. Depending on its location, pain may feel worse in certain positions, like when sneezing or coughing or with movements like rotation or looking upwards.
Stiffness is a common symptom, which can vary with weather changes. Too little as well as too much activity can be a problem, but the BEST way to self-manage CS is to keep active! Range of motion exercises, strength training, and walking all help reduce the symptoms of CS.