These muscles are located in the groin. The longus originates on the pubic body just below the pubic crest and inserts on the middle third of the linea aspera.The brevis muscle originates on the inferior ramus and body of the pubis and has its attachment to the lesser trochanter and linea aspera of the femur. Trigger points in these muscles are the most common muscular cause of groin pain. Distal trigger points refer pain to the upper medial knee and down the tibia. Proximal trigger points refer into the anterior hip area.
Leg Pain
Trigger points in the iliopsoas muscle
This muscle originates on the bodies and disks of T12-L5 and the inner ilium. It inserts on the lesser trochanter of the femur. The psoas flexes the hip when the spine is fixed. When the leg is fixed it extends the lumbar spine increasing lumbar lordosis. This Muscle is often chronically shortened due to inactivity and sitting posture. When trigger points are present they will refer pain primarily to the lower lumbar area and the sacrum as well as into the anterior thigh. Trigger points in the iliopsoas muscle can mimic appendicitis.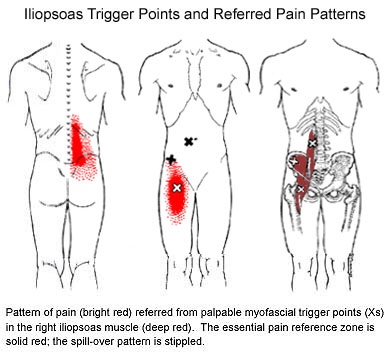
Trigger points in the piriformis muscle
The piriformis muscle is a small muscle deep to glute max and lies over top of the sciatic nerve. It originates on the anterior sacrum, and inserts on the greater trochanter of the femur. It’s main action is to laterally rotate the femur. When trigger points developed in this muscle they will refer pain into the sacro-iliac region, across the posterior hip and down the leg. This muscle can also be a cause of sciatic nerve irritation if it gets tight, causing “sciatica” symptoms. 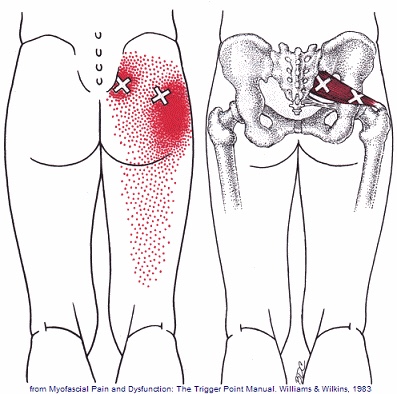
Trigger points in the gluteus minimus
The gluteus minimus is a small but important muscle that lies deep to the gluteus medius. It originates on the gluteal surface of the ilium, and attaches on the greater trochanter of the femur. It’s main actions are to abduct and medically rotate the hip. Trigger points in this muscle refer pain into the buttock and down the lateral and posterior leg, mimicking sciatica. This muscle should be the first to be examined if a straight leg test turns out negative. 
Pathophysiology of trigger points.
A large number of factors have been identified as causes of trigger point activation. These include acute or chronic overload of muscle tissue, disease, psychological distress, systemic inflammation, homeostatic imbalances, direct trauma, radiculopathy, infections, and lifestyle choices such as smoking. Trigger points form as a local contraction of muscle fibres in a muscle or bundle of muscle fibres. These can pull on ligaments and tendons associated with the muscle which can cause pain to be felt deep inside a joint. It is theorized that trigger points form from excessive release of acetylcholine causing sustained depolarization of muscle fibres. Trigger points present an abnormal biochemical composition with elevated levels of acetylcholine, noradrenaline and serotonin and a lower ph. The contracted fibres in a trigger point constricts blood supply to the area creating an energy crisis in the tissue that results in the production of sensitizing substances that interact with pain receptors producing pain. When trigger points are present in a muscle there is often pain and weakness in the associated structures. These pain patterns follow specific nerve pathways that have been well mapped to allow for accurate diagnosis or the causative pain factor.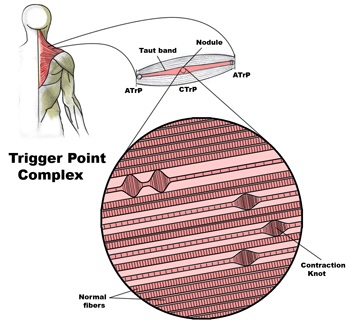
Diagnosis of trigger points.
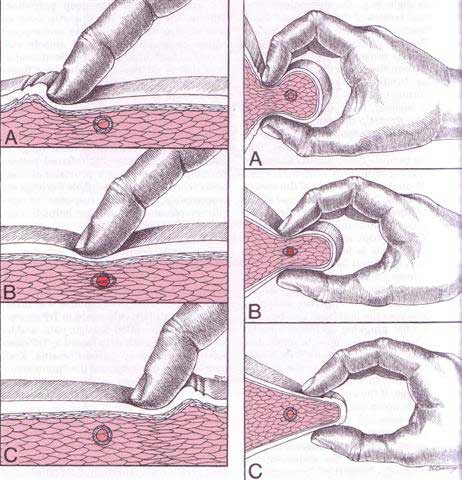
Diagnosis of trigger points typically takes into account symptoms, pain patterns, and manual palpation. When palpating the therapist will feel for a taut band of muscle with a hard nodule within it. Often a local twitch response will be elicited by running a finger perpendicular to the muscle fibres direction. Pressure applied to the trigger point will often reproduce the pain complaint of the patient and the referral pattern of the trigger point. Often there is a heat differential in the local area of the trigger point. 
What is a trigger point
Dr Janet travel coined the term trigger point in 1942 to describe clinical findings with characteristics of pain related a discrete irritable point in muscle or fascia that was not caused by acute trauma, inflammation, degeneration, neoplasm or infection. The painful point can be palpated as a nodule or tight band in the muscle that can produce a local twitch response when stimulated. Palpation of the trigger point reproduces the pain and symptoms of the patient and the pain radiates in a predictable referral pattern specific to the muscle harbouring the trigger point.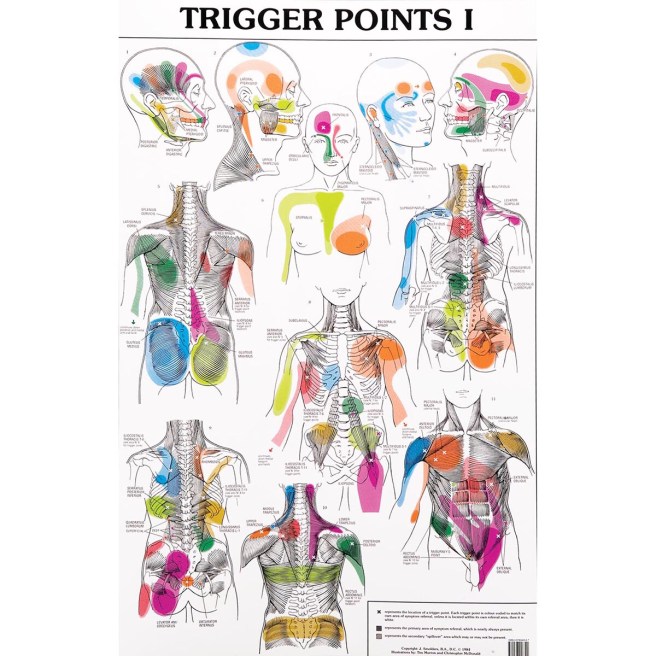
What to expect with a trigger point massage.
A treatment with Bryan is very user friendly. And, no, you don’t have to remove any clothing. However, bringing a t-shirt and a pair of shorts or sweats is recommended.
The first time you come for a treatment you will be asked to fill out a Client History form. Bryan will go over the information you provide, asking for more detail and discussing the type of pain you are having and its location.
The treatment itself involves locating the Trigger Points in the muscle or soft tissue and applying a deep focused pressure to the Point. This will reproduce the pain and the referral pattern that is characteristic of that pain.
The treatment will be uncomfortable at first, but as the Trigger Points release, the pain will decrease. The pressure will always be adjusted to your tolerance level. If, at any time, you feel too uncomfortable you can ask Bryan to ease off a bit.
Depending on your specific problem, Bryan may also use some stretching and / or range-of-motion techniques, as needed.
After treatment, it is usually recommended that the client apply moist heat to the area treated.
Our Condition of the Month: ITB Syndrome
Iliotibial Band Syndrome
Your iliotibial band is a fibrous band of tissue running from the crest of your hip, down to your knee. A muscle near the crest of your hip called the tensor fascia lata, attaches to this band to help control movements of your leg. Your iliotibial band passes over the point of your hip and over another bony bump on the outside of your knee called the lateral epicondyle. When the band is too tight, it can become painfully inflamed as it repeatedly rubs over the top of either of these bony projections. Irritation at the bony bump near the knee is called iliotibial band friction syndrome.
The condition usually presents as pain on the outside of your knee that becomes worse with repetitive knee flexion or extension. This condition is the leading cause of lateral knee pain in runners, especially slower “joggers.” The pain usually develops 10-15 minutes into the workout. You may sometimes feel or hear a click during movement. Symptoms generally ease at rest. Running on slick “wintry” surfaces may aggravate the condition. Excessively worn running shoes may be a culprit.
This problem is commonly caused by weakness in your gluteal muscles. When these muscles are weak, the muscle that attaches to your iliotibial band must contract harder to stabilize your hip. Having one leg longer than another is a known aggravating factor.
Runners should minimize downhill running and avoid running on a banked surface like the crown of a road or indoor track, as well as wet or icy surfaces. Runners should reverse directions on a circular track at least each mile. Bicyclists may need to adjust seat height and avoid “toe in” pedal positions. Avoid using stair climbers or performing squats and dead lifts. Sports cream and home ice massage may provide some relief of symptoms.
Our Exercise Of The Month: ITB Foam Roller
- Lie on your side with your affected thigh over a foam roll.
- Lift your shoulders off of the floor with your arm and roll the fleshy part your mid & lower thigh back and forth over the foam roller.
- Avoid rolling over the bony point of your hip unless specifically directed.
- Perform this exercise for one minute twice per day or as directed.
