Patellofemoral pain syndrome (PFPS), also called “Runners Knee”, describes the symptom complex of knee discomfort, swelling, or crepitus that results from excessive or imbalanced forces acting on the joint. It is the most common cause of knee pain in the general population, affecting an estimated 25% of adults.
PFPS is most commonly related to lateral tracking of the patella. The patella has a natural tendency to migrate laterally due to the pull of the quadriceps and the slight natural valgus of the lower extremity. A new study in the Journal of Sports Medicine (1) provides additional confirmation that when managing patellofemoral pain syndrome, clinicians must address two critical yet often overlooked issues.
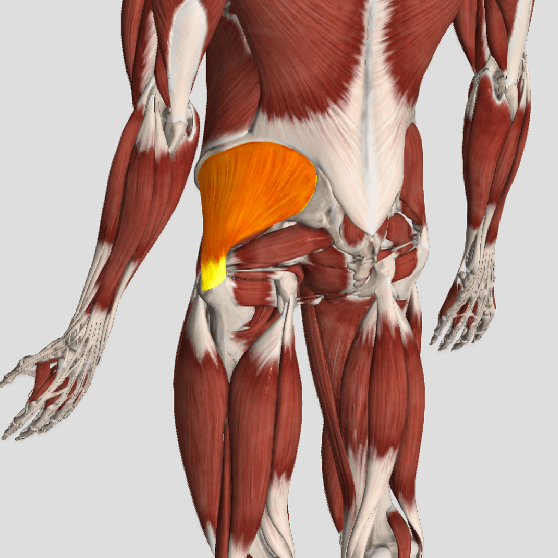
This study concludes that PFPS and dynamic knee valgus do not arise primarily from knee dysfunction, rather from hip abductor/ external rotator weakness and/or foot hyperpronation.
“The most effective intervention programs included exercises targeting the hip external rotator and abductor muscles and knee extensor muscles.” and “PFPS patients with foot abnormalities, such as those with increased rearfoot eversion or pes pronatus, may benefit the most from foot orthotics.”
Since gluteus medius and VMO weakness are key factors in the development of PFPS, strengthening exercises that target those muscles prove most effective. Stabilization exercises may include pillow push (push the back of your knee into a pillow for 5-6 seconds), supine heel slide, terminal knee (short-arc) extension, clam, glut bridge, semi-stiff deadlift, posterior lunge, and monster walk.
Myofascial release and stretching should be directed at hypertonic muscles, including the TFL, gastroc, soleus, hamstring, piriformis, hip rotators, and psoas. Myofascial release or IASTM may be appropriate for tightness in the iliotibial band, vastus lateralis, posterior hip capsule, and lateral knee retinaculum.
Manipulation may be necessary for restrictions in the lumbosacral and lower extremity joints. Hypermobility is common in the ipsilateral SI joint with restrictions present contralaterally. Evidence has shown that patellar tracking braces, i.e. BioSkin® or PatellaPro®, may lead to better outcomes.
Lifestyle modification may be necessary to reduce pain-provoking endeavors, especially running, jumping and other activities that induce a valgus stress. Athletes should avoid allowing their knee to cross in front of their toes while squatting. Arch supports or custom orthotics may be necessary to correct hyperpronation. Runners should avoid cross-over gaits and change shoes every 250 to 500 miles.
.
.
.
.
.
.
.
#pain
#kneepain
#chiropractic
#fitness
#sports
#wellness
#fitness
#healthyliving
#healthychoices
#Winnipeg
References
1. Petersen W, Rembitzki I, Liebau C. Patellofemoral pain in athletes. Open Access Journal of Sports Medicine. 2017;8:143-15