The piriformis muscle is a small muscle deep to glute max and lies over top of the sciatic nerve. It originates on the anterior sacrum, and inserts on the greater trochanter of the femur. It’s main action is to laterally rotate the femur. When trigger points developed in this muscle they will refer pain into the sacro-iliac region, across the posterior hip and down the leg. This muscle can also be a cause of sciatic nerve irritation if it gets tight, causing “sciatica” symptoms. 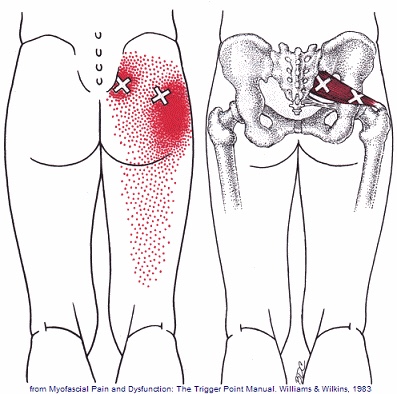
Hip Pain
Piriformis Syndrome; a real bummer.
Piriformis syndrome results from compression of the sciatic nerve as it passes underneath a muscle in your buttock called the piriformis. Your piriformis muscle attaches from the lowest part of your spine (sacrum) and travels across to your hip. The muscle helps to rotate your leg outward when it contracts. In most people, the sciatic nerve travels deep to the piriformis muscle.

When your piriformis muscle is irritated or goes into spasm, it may cause a painful compression of your sciatic nerve. Approximately ¼ of the population is more likely to suffer from piriformis syndrome because their sciatic nerve passes through the muscle.
Piriformis syndrome may begin suddenly as a result of an injury or may develop slowly from repeated irritation. Common causes include: a fall onto the buttocks, catching oneself from a “near fall,” strains, long distance walking, stair climbing or sitting on the edge of a hard surface or wallet. In many cases, a specific triggering event cannot be pinpointed. The condition is most common in 40-60 year olds and affects women more often than men.
Symptoms of piriformis syndrome include pain, numbness or tingling that begins in your buttock and radiates along the course of your sciatic nerve toward your foot. Symptoms often increase when you are sitting or standing in one position for longer than 15-20 minutes. Changing positions may help. You may notice that your symptoms increase when you walk, run, climb stairs, ride in a car, sit cross-legged or get up from a chair.
Sciatic arising from piriformis syndrome is one of the most treatable varieties and generally is relieved by the type of treatment provided in this office. You may need to temporarily limit activities that aggravate the piriformis muscle, including hill and stair climbing, walking on uneven surfaces, intense downhill running or twisting and throwing objects backwards, i.e., firewood. Be sure to avoid sitting on one foot and take frequent breaks from prolonged standing, sitting and car rides. You may find relief by applying an ice pack to your buttock for 15-20 minutes at a time, several times throughout the day.
Trigger points in the gluteus minimus
The gluteus minimus is a small but important muscle that lies deep to the gluteus medius. It originates on the gluteal surface of the ilium, and attaches on the greater trochanter of the femur. It’s main actions are to abduct and medically rotate the hip. Trigger points in this muscle refer pain into the buttock and down the lateral and posterior leg, mimicking sciatica. This muscle should be the first to be examined if a straight leg test turns out negative. 
Lower Crossed Syndrome

Your posture plays an important role in your overall health. Poor posture leads to chronic strain and discomfort. “Lower crossed syndrome” is poor posture that results from excessive tightness in your lower back and hip flexor muscles with weakness in your abdominal and buttock muscles. Patients with lower crossed syndrome often have a “sway back.” Patients who sit for prolonged periods of time are at greater risk of lower crossed syndrome.
This postural problem commonly leads to painful conditions involving the back or hips. Successful treatment of lower cross syndrome involves stretching excessively tight muscles, strengthening weak muscles, taking frequent breaks from sitting, and modifying your workstation to be more user friendly.
Foot Over Pronation

The normal walking or running cycle begins with your heel striking the ground. As you transfer your body weight onto the front part of your foot, the arch of your foot naturally flattens slightly. This is called pronation.
The tissues that help maintain the arch of your foot are exposed to tremendous stress and may eventually break down. The loss of the normal arch of your foot results in a condition called “overpronation” or flat feet. This condition most commonly develops over a long period of time from repetitive stress.
Overpronation by itself is not painful, but the problem often leads to secondary problems, which may be painful. Plantar fasciitis, foot pain, shin splints and problems in the knee, hip or lower back are all related to overpronation. Patients who carry excess weight are more likely to develop this condition.
To help support your foot, you should wear shoes with good arch supports consistently. In some cases, specially molded orthotics may be needed to help support your arch.
Trigger points in the gluteus medius muscle
The gluteus medius muscle plays an important role in hip and pelvic stability. It originates on the gluteal surface of the ilium, deep to the gluteus Maximus. It inserts on the greater trochanter of the femur. It’s main actions are to abduct the hip and to assist in internal rotation of the hip. It also maintains pelvic stability during walking and running. Trigger points in this muscle will refer pain into the sacrum, the iliac crest, and down the lateral hip and into the thigh. This muscle is often a cause of lower pack pain.
Trigger points in the gluteus Maximus
The gluteus Maximus is the buttock muscle. It originates on the gluteal surface of the ilium, lumbar fascia, sacrum and sacrotuberous ligament. It inserts on the gluteal tuberosity of the femur and the iliotibial tract. Extension and lateral rotation of the hip are it’s main actions. This muscle is heavily involved in activities like ice skating and is a common area to develops trigger points. When trigger points do develop they can refer pain in a crescent pattern from the gluteal fold to the sacrum. Trigger points can also refer pain deep into the buttock itself making it feel like other deeper muscles are involved. These symptoms can sometimes be mistaken for s.i. Joint problems. 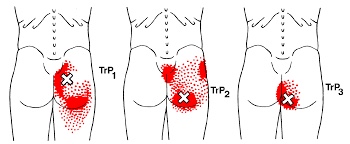
SI Joint Dysfunction. Nothing FUN about it.
Your sacroiliac joint is the mechanical link on each side of your hip that connects your legs to the rest of your body. The joint has a limited but very important degree of mobility. Symptoms develop when one or both of the joints loses normal motion. When a joint becomes “restricted”, a self-perpetuating cycle of discomfort follows. Restriction causes the muscles to become overworked, leading to tightness, compression, inflammation, pain and more restriction.
 Sacroiliac problems can happen as a result of repetitive strenuous activity or trauma- like a fall onto the buttocks. Other causes of sacroiliac joint problems include, poor posture, having one leg slightly longer than another, having an altered gait, having flat feet or scoliosis, or having pain somewhere else in your legs. Pregnancy is a common trigger for sacroiliac joint problems due to weight gain, gait changes and postural stress.
Sacroiliac problems can happen as a result of repetitive strenuous activity or trauma- like a fall onto the buttocks. Other causes of sacroiliac joint problems include, poor posture, having one leg slightly longer than another, having an altered gait, having flat feet or scoliosis, or having pain somewhere else in your legs. Pregnancy is a common trigger for sacroiliac joint problems due to weight gain, gait changes and postural stress.
Sacroiliac joint problems often begin as a focal discomfort in your back just below the belt line, slightly to one side of center. Your pain can travel into your buttock or thigh. Symptoms are often worse by standing on the affected side. The pain may become more apparent when you change positions- like exiting a chair, car or bed, or during long car rides. The pain is often relieved by lying down.
To assist with your recovery, you should avoid any activity that provokes pain, like standing on the affected leg or prolonged sitting.
My ankle hurts…….
The posterior tibialis muscle begins deep in your calf. The muscle is connected to the arch of your foot by a tendon that runs along the inside of your ankle, just behind the large bump called the medial malleolus. When you walk, the posterior tibialis muscle lifts the arch of your foot. 
Posterior tibial tendon dysfunction is one of the most common foot and ankle problems. The tendon may be damaged from an acute injury, like an accident or fall. More commonly, problems arise from overuse or repeated strain. Ongoing irritation slowly damages the tendon’s fibers and eventually leads to weakening and degeneration. This decreases the tendon’s ability to support your foot when you walk. As the tendon becomes less effective, the arch of your foot is allowed to collapse, which further increases the strain on the muscle and tendon.
The condition is often triggered from overuse and/or training on excessively hard surfaces. Other factors that can contribute to posterior tibial tendon dysfunction include: obesity, diabetes, hypertension, prior surgery or steroid injections.
Symptoms include pain or swelling along the course of the tendon, particularly behind your inner ankle bone. Symptoms often begin following an increase in training intensity or duration. Standing, walking, or running will likely increase your discomfort. Your pain may be aggravated by spending prolonged periods of time on your feet, especially, when standing tiptoe and walking stairs or uneven surfaces.
Early diagnosis and treatment is important to slow progression of the disorder. You may need to temporarily limit weight-bearing activity to allow your tendon to heal. Using a stationary cycle, elliptical machine, or swimming can be good alternatives to walking and running. Your doctor will likely prescribe arch supports or orthotics to help support your foot. You will be given exercises to strengthen the posterior tibialis muscle. These exercises should be performed while wearing shoes with good arch supports. In certain instances, a walking cast or boot may be needed to temporarily protect your foot.
Hip Abductor Weakness

One very important job of your hip muscles is to maintain the alignment of your leg when you move. One of the primary hip muscles, the gluteus medius, plays an especially important stabilizing role when you walk, run, or squat. The gluteus medius attaches your thigh bone to the crest of your hip. When you lift your left leg, your right gluteus medius must contract in order to keep your body from tipping toward the left. And when you are standing on a bent leg, your gluteus medius prevents that knee from diving into a “knock knee” or “valgus” position.
Weakness of the gluteus medius allows your pelvis to drop and your knee to dive inward when you walk or run. This places tremendous strain on your hip and knee and may cause other problems too. When your knee dives inward, your kneecap is forced outward, causing it to rub harder against your thigh bone- creating a painful irritation and eventually arthritis. Walking and running with a relative “knock knee” position places tremendous stress on the ligaments around your knee and is a known cause of “sprains”. Downstream, a “knock knee” position puts additional stress on the arch of your foot, leading to other painful problems, like plantar fasciitis. Upstream, weak hips allow your pelvis to roll forward which forces your spine into a “sway back” posture. This is a known cause of lower back pain. Hip muscle weakness seems to be more common in females, especially athletes.
You should avoid activities that cause prolonged stretching of the hip abductors, like “hanging on one hip” while standing, sitting crossed legged, and sleeping in a side-lying position with your top knee flexed and touching the bed. Patients with fallen arches may benefit from arch supports or orthotics. Obesity causes more stress to the hip muscles, so overweight patients may benefit from a diet and exercise program. The most important treatment for hip abductor weakness is strength training. Hip strengthening is directly linked to symptom improvement. Moreover, people with stronger hip muscles are less likely to become injured in the first place.
