Pregnancy and Low Back Pain?




Patellofemoral pain syndrome (PFPS), also called “Runners Knee”, describes the symptom complex of knee discomfort, swelling, or crepitus that results from excessive or imbalanced forces acting on the joint. It is the most common cause of knee pain in the general population, affecting an estimated 25% of adults.
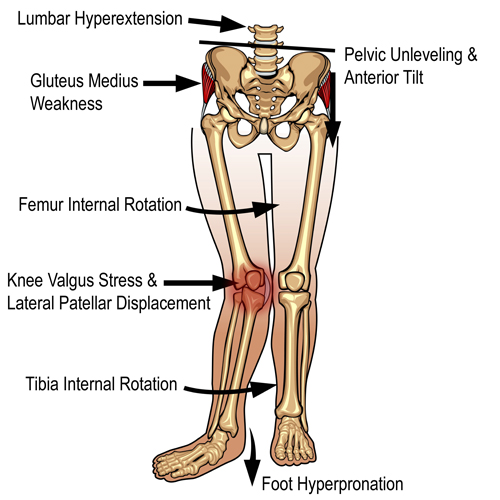
PFPS is most commonly related to lateral tracking of the patella. The patella has a natural tendency to migrate laterally due to the pull of the quadriceps and the slight natural valgus of the lower extremity. A new study in the Journal of Sports Medicine (1) provides additional confirmation that when managing patellofemoral pain syndrome, clinicians must address two critical yet often overlooked issues.
This study concludes that PFPS and dynamic knee valgus do not arise primarily from knee dysfunction, rather from hip abductor/ external rotator weakness and/or foot hyperpronation.
“The most effective intervention programs included exercises targeting the hip external rotator and abductor muscles and knee extensor muscles.” and “PFPS patients with foot abnormalities, such as those with increased rearfoot eversion or pes pronatus, may benefit the most from foot orthotics.”
Since gluteus medius and VMO weakness are key factors in the development of PFPS, strengthening exercises that target those muscles prove most effective. Stabilization exercises may include pillow push (push the back of your knee into a pillow for 5-6 seconds), supine heel slide, terminal knee (short-arc) extension, clam, glut bridge, semi-stiff deadlift, posterior lunge, and monster walk.
Myofascial release and stretching should be directed at hypertonic muscles, including the TFL, gastroc, soleus, hamstring, piriformis, hip rotators, and psoas. Myofascial release or IASTM may be appropriate for tightness in the iliotibial band, vastus lateralis, posterior hip capsule, and lateral knee retinaculum.
Manipulation may be necessary for restrictions in the lumbosacral and lower extremity joints. Hypermobility is common in the ipsilateral SI joint with restrictions present contralaterally. Evidence has shown that patellar tracking braces, i.e. BioSkin® or PatellaPro®, may lead to better outcomes.
Lifestyle modification may be necessary to reduce pain-provoking endeavors, especially running, jumping and other activities that induce a valgus stress. Athletes should avoid allowing their knee to cross in front of their toes while squatting. Arch supports or custom orthotics may be necessary to correct hyperpronation. Runners should avoid cross-over gaits and change shoes every 250 to 500 miles.
.
.
.
.
.
.
.
#pain
#kneepain
#chiropractic
#fitness
#sports
#wellness
#fitness
#healthyliving
#healthychoices
#Winnipeg
References
1. Petersen W, Rembitzki I, Liebau C. Patellofemoral pain in athletes. Open Access Journal of Sports Medicine. 2017;8:143-15

Becoming healthy and staying healthy is hard, challenging work but worth every second of persistence.

Moving is good for your back and muscles, especially if you have back pain.

Acupuncture is a centuries-old healing practice that originated in ancient China and has since gained popularity worldwide for its effectiveness in treating a wide range of health conditions. But how exactly does acupuncture work? In this article, we’ll explore the science behind acupuncture and shed light on its mechanisms of action.
Understanding Traditional Chinese Medicine
Before delving into the scientific aspects of acupuncture, it’s important to understand the principles of Traditional Chinese Medicine (TCM) upon which it is based. According to TCM theory, the body’s vital energy, known as Qi (pronounced “chee”), flows through meridians or pathways in the body. When the flow of Qi is disrupted or blocked, illness and pain can result.
Acupuncture Points and Meridians
Acupuncture involves the insertion of thin needles into specific points on the body known as acupuncture points or acupoints. These points are located along the meridians and are believed to correspond to different organs and functions in the body. By stimulating these points, acupuncturists aim to restore the balance and flow of Qi, promoting healing and well-being.
Scientific Explanations for Acupuncture
While the concepts of Qi and meridians may seem abstract to some, modern research has provided scientific explanations for the effects of acupuncture. Here are some of the key mechanisms by which acupuncture is believed to work:
1. Stimulation of Nerve Endings: Acupuncture needles stimulate nerve endings in the skin and muscles, sending signals to the brain. This can trigger the release of neurotransmitters such as endorphins and serotonin, which have pain-relieving and mood-enhancing effects.
2. Modulation of Neurotransmitters: Acupuncture has been shown to influence the levels of various neurotransmitters in the brain, including opioid peptides, which are natural painkillers produced by the body. By modulating these neurotransmitters, acupuncture can help regulate pain perception and mood.
3. Regulation of Blood Flow: Acupuncture can affect blood flow to specific areas of the body, promoting circulation and delivering oxygen and nutrients to tissues. Improved blood flow can aid in the healing process and reduce inflammation and pain.
4. Activation of the Autonomic Nervous System: Acupuncture has been found to activate the autonomic nervous system, which controls involuntary bodily functions such as heart rate, digestion, and immune response. This activation can have widespread effects on various physiological processes in the body.
5. Regulation of Neuroendocrine Pathways: Acupuncture can influence the release of hormones and other signaling molecules involved in the body’s stress response and immune function. By regulating these neuroendocrine pathways, acupuncture can help restore balance and promote health.
In conclusion, acupuncture may have ancient roots, but its efficacy is supported by modern scientific research. By stimulating specific points on the body, acupuncture can trigger a variety of physiological responses that promote healing and alleviate symptoms. Whether you’re seeking relief from pain, stress, or other health concerns, acupuncture offers a safe and effective treatment option backed by both tradition and science.

Headaches are a prevalent ailment affecting people of all ages and backgrounds, often causing discomfort and disrupting daily activities. While headaches can stem from various causes, understanding their different types and exploring holistic treatments like chiropractic care can offer relief and long-term solutions. In this blog post, we’ll delve into the most common types of headaches and how chiropractic techniques can help alleviate their symptoms.
Tension headaches are the most common type, characterized by a dull, aching pain that wraps around the head. They often result from stress, muscle tension in the neck and shoulders, poor posture, or jaw clenching.
How Chiropractic Can Help: Chiropractic adjustments target misalignments in the spine and neck, which can alleviate muscle tension and improve posture. By restoring proper alignment, chiropractic care reduces the frequency and intensity of tension headaches, providing long-term relief.
Migraines are intense, throbbing headaches often accompanied by symptoms such as nausea, sensitivity to light and sound, and visual disturbances. They can be triggered by various factors, including hormonal changes, certain foods, stress, and environmental factors.
How Chiropractic Can Help: Chiropractic adjustments, particularly those targeting the cervical spine, can reduce nerve irritation and improve blood flow to the brain. Additionally, chiropractors may recommend dietary modifications, stress management techniques, and lifestyle changes to help prevent migraine attacks and reduce their severity.
Cluster headaches are excruciatingly painful headaches that occur in clusters or cycles, typically around the same time each day or night. They often affect one side of the head and are accompanied by symptoms such as eye redness, tearing, and nasal congestion.
How Chiropractic Can Help: Chiropractic adjustments can help relieve pressure on the nerves and blood vessels in the neck and head, reducing the frequency and intensity of cluster headaches. Additionally, chiropractors may recommend lifestyle changes and relaxation techniques to manage stress and minimize triggers.
Cervicogenic headaches originate from structural problems in the neck, such as misaligned vertebrae, muscle tightness, or joint dysfunction. The pain typically starts in the neck and radiates to the head, often mimicking the symptoms of tension headaches or migraines.
How Chiropractic Can Help: Chiropractic adjustments target the underlying issues in the cervical spine, addressing misalignments and restoring proper function. By improving spinal alignment and reducing nerve irritation, chiropractic care effectively treats cervicogenic headaches and prevents their recurrence.
Sinus headaches result from inflammation or congestion in the sinus cavities, often due to allergies, sinus infections, or environmental irritants. The pain is usually localized around the forehead, cheeks, and eyes and may worsen with changes in air pressure or temperature.
How Chiropractic Can Help: While chiropractic care does not directly treat sinus inflammation, it can help alleviate associated neck and shoulder tension. By improving spinal alignment and reducing muscle tightness, chiropractic adjustments can alleviate secondary headaches caused by sinus issues, providing symptomatic relief.
Headaches can be debilitating, affecting every aspect of daily life. However, chiropractic care offers a holistic approach to headache management, addressing underlying issues in the spine and neck to provide natural and effective relief. Whether you suffer from tension headaches, migraines, cluster headaches, cervicogenic headaches, or sinus headaches, chiropractic techniques can help alleviate pain, improve spinal function, and enhance overall well-being. Consult with a qualified chiropractor to develop a personalized treatment plan tailored to your specific needs and experience the transformative benefits of chiropractic care in managing headaches.

Recovering from an injury can be a challenging and often frustrating journey. While many individuals are eager to return to their regular routines, doing so without proper guidance can lead to further harm and prolonged recovery. This is where the expertise of a personal trainer becomes invaluable. Personal trainers provide tailored support and guidance, ensuring a safe and effective rehabilitation process. Here are key reasons why people with injuries should consider working with a personal trainer:
Personal trainers assess your specific injury, fitness level, and overall health to create a personalized rehabilitation plan. They design exercises that target the injured area, promoting healing while avoiding movements that could exacerbate the injury. This customized approach ensures that every workout is both safe and beneficial.
Certified personal trainers have extensive knowledge of human anatomy, biomechanics, and injury rehabilitation. They understand the complexities of different injuries and the most effective methods for recovery. Their expertise allows them to select appropriate exercises and modifications, reducing the risk of further injury and speeding up the healing process.
One of the most critical aspects of exercising with an injury is maintaining proper technique and form. Personal trainers provide hands-on instruction and continuous feedback, ensuring that you perform each exercise correctly. This attention to detail helps prevent compensation patterns and incorrect movements that could hinder recovery or cause new injuries.
Recovery from an injury is a dynamic process that requires ongoing assessment and adjustment. Personal trainers monitor your progress closely, making necessary modifications to your program based on your healing and feedback. This adaptive approach ensures that your rehabilitation plan evolves with your recovery, maximizing effectiveness and safety.
Rehabilitating an injury can be mentally and physically taxing. Personal trainers offer invaluable motivation and emotional support, helping you stay committed to your recovery plan. Their encouragement and positive reinforcement can boost your confidence and keep you focused on your goals, even during challenging times.
Returning to your regular exercise routine or daily activities too quickly can lead to setbacks. Personal trainers guide you through a safe and gradual transition, ensuring that your body is adequately prepared for increased activity levels. They help bridge the gap between rehabilitation and full recovery, reducing the likelihood of re-injury.
Personal trainers educate clients on proper techniques, body mechanics, and lifestyle choices that can prevent future injuries. They teach you how to listen to your body, recognize early signs of strain, and incorporate preventive measures into your fitness routine. This proactive approach promotes long-term health and reduces the risk of recurrent injuries.
Beyond injury rehabilitation, personal trainers take a holistic approach to your health and wellness. They consider factors such as nutrition, sleep, stress management, and overall fitness, all of which play crucial roles in recovery and injury prevention. By addressing these aspects, trainers help you achieve optimal health and well-being.
Working with a personal trainer can be a transformative experience for individuals recovering from injuries. The combination of personalized rehabilitation programs, expert knowledge, proper technique instruction, progress monitoring, motivation, safe transitions, education on injury prevention, and holistic health support creates an ideal environment for recovery. If you’re dealing with an injury and looking to regain your strength and functionality, partnering with a personal trainer could be the key to a successful and sustainable recovery. Prioritize your health and take the first step toward healing with the guidance of a skilled personal trainer.