A large number of factors have been identified as causes of trigger point activation. These include acute or chronic overload of muscle tissue, disease, psychological distress, systemic inflammation, homeostatic imbalances, direct trauma, radiculopathy, infections, and lifestyle choices such as smoking. Trigger points form as a local contraction of muscle fibres in a muscle or bundle of muscle fibres. These can pull on ligaments and tendons associated with the muscle which can cause pain to be felt deep inside a joint. It is theorized that trigger points form from excessive release of acetylcholine causing sustained depolarization of muscle fibres. Trigger points present an abnormal biochemical composition with elevated levels of acetylcholine, noradrenaline and serotonin and a lower ph. The contracted fibres in a trigger point constricts blood supply to the area creating an energy crisis in the tissue that results in the production of sensitizing substances that interact with pain receptors producing pain. When trigger points are present in a muscle there is often pain and weakness in the associated structures. These pain patterns follow specific nerve pathways that have been well mapped to allow for accurate diagnosis or the causative pain factor.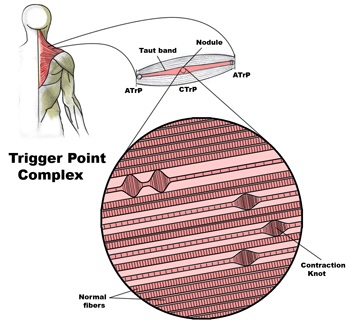
Car Accident
Diagnosis of trigger points.
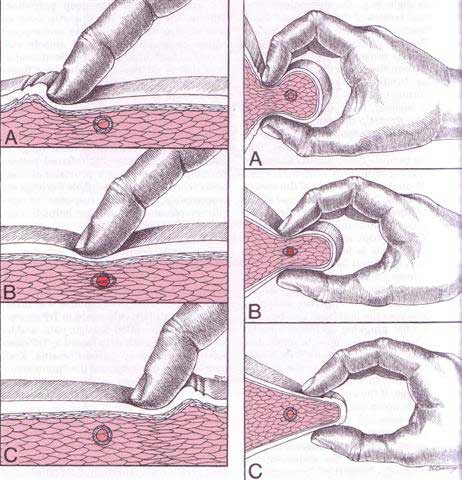
Diagnosis of trigger points typically takes into account symptoms, pain patterns, and manual palpation. When palpating the therapist will feel for a taut band of muscle with a hard nodule within it. Often a local twitch response will be elicited by running a finger perpendicular to the muscle fibres direction. Pressure applied to the trigger point will often reproduce the pain complaint of the patient and the referral pattern of the trigger point. Often there is a heat differential in the local area of the trigger point. 
Do I have a cuff tear?
One of the most common causes of shoulder pain is a rotator cuff (RC) tear. To determine just how common this is, one study looked at a population of 683 people regardless of whether or not they had shoulder complaints. There were 229 males and 454 females for a total of 1,366 shoulders. (The participants’ average age was 58 years, ranging from 22 to 87 years old.)
The research team found 20.7% had full thickness rotator cuff tears. Of those with shoulder pain, only 36% had tears found on ultrasound. Of those without shoulder pain, 17% also had tears! Risk factors for an increased for tearing of the rotator cuff include a history of trauma, the dominant arm (ie your right arm if you’re right handed), and increasing age.
In a review of radiologic studies of 2,553 shoulders, researchers found full-thickness rotator cuff tears in 11.75% and partial thickness tears in 18.49% of the subjects for a total of 30.24% having some degree of tearing. In this group, about 40% of tears were found in pain-free shoulders. The researchers concluded that rotator cuff tears are common and frequently asymptomatic.
Both of these studies support the necessity to FIRST consider the patient’s clinical presentation and then correlate that with the imaging results. In other words, the presence of a RC tear on an image (usually MRI or ultrasound) does NOT necessarily mean there is pain (and vise versa)!
So what other things could be causing the shoulder pain? There are many: impingement, tendonitis, bursitis, muscle strain, capsular (and other ligament) sprain, frozen shoulder, and osteoarthritis (the “wearing out” type). Also, rheumatoid arthritis, lupus, polymyalgia rheumatica and other autoimmune types of “arthropathies,” fibromyalgia, a herniated cervical disk, shoulder dislocations, whiplash injuries, and more!
Most importantly, we must NOT forget to include referred pain to the shoulder from an impaired heart (such as coronary heart disease or heart attack), lung, liver, or gall bladder as these problems commonly refer pain to the shoulder and may represent a MEDICAL EMERGENCY!
What to expect with a trigger point massage.
A treatment with Bryan is very user friendly. And, no, you don’t have to remove any clothing. However, bringing a t-shirt and a pair of shorts or sweats is recommended.
The first time you come for a treatment you will be asked to fill out a Client History form. Bryan will go over the information you provide, asking for more detail and discussing the type of pain you are having and its location.
The treatment itself involves locating the Trigger Points in the muscle or soft tissue and applying a deep focused pressure to the Point. This will reproduce the pain and the referral pattern that is characteristic of that pain.
The treatment will be uncomfortable at first, but as the Trigger Points release, the pain will decrease. The pressure will always be adjusted to your tolerance level. If, at any time, you feel too uncomfortable you can ask Bryan to ease off a bit.
Depending on your specific problem, Bryan may also use some stretching and / or range-of-motion techniques, as needed.
After treatment, it is usually recommended that the client apply moist heat to the area treated.
He barely hit me; why does it hurt?
You may have heard the comment, “If there’s no damage to the car, then there’s no injury.” Unfortunately, that does not always seem to be the case.
There are MANY factors that affect the dynamics of a collision and whether or not injury occurs. A short list includes: vehicle type and design, speed, angle of collision, momentum, acceleration factors, friction, kinetic and potential energy, height, weight, muscle mass, seat back angle and spring, head position upon impact, etc.
Consider Sir Isaac Newton’s Third Law of Motion: “For every action there is an equal and opposite reaction.” This law applies to a car accident at any speed. Using the analogy of hitting a pool ball into the corner pocket straight on, when the cue ball stops, its momentum is transferred to the target ball which accelerates at the same speed…hopefully into the corner pocket!
What evidence do we have of whiplash?
Whiplash, or WAD (Whiplash Associated Disorders), refers to a neck injury where the normal range of motion is exceeded, resulting in injury to the soft-tissues (hopefully with no fractures) in the cervical region. There are a LOT of factors involved that enter into the degree of injury and length of healing time. Let’s take a closer look!
Picture the classic rear-end collision. The incident itself may be over within 300 milliseconds (msec), which is why it’s virtually impossible to brace yourself effectively for the crash as a typical voluntary muscle contraction takes two to three times longer (800-1000 msec) to accomplish.
In the first 50 msec, the force of the rear-end collision pushes the vehicle (and the torso of the body) forwards leaving the head behind so the cervical spine straightens out from its normal “C-shape” (or lordosis). By 75-100 msec, the lower part of the neck extends or becomes more C-shaped while the upper half flexes or moves in an opposite direction creating an “S” shape to the neck. Between 150-200msec, the whole neck hyper extends and the head may hit the head rest IF the headrest is positioned properly. In the last 200-300 msec, the head is propelled forwards into flexion in a “crack the whip” type of motion.
Injury to the neck may occur at various stages of this very fast process, and many factors determine the degree of injury such as a smaller car being hit by a larger car, the impact direction, the position of the head upon impact (worse if turned), if the neck is tall and slender vs. short and muscular, the angle and “springiness” of the seat back and relative position of the headrest, dry vs. wet/slippery pavement, and airbag deployment, just to name a few.
Some other factors that can predict recovery include: limited neck motion, the presence of neurological loss (nerve specific muscle weakness and/or numbness/tingling), high initial pain levels (>5/10 on a 0-10 scale), high disability scores on questionnaires, overly fearful of harming oneself with usual activity and/or work, depressive symptoms, post-traumatic stress, poor coping skills, headaches, back pain, widespread or whole body pain, dizziness, negative expectation of recovery, pending litigation, catastrophizing, age (older is worse), and poor pre-collision health (both mental and physical).
Research shows the best outcomes occur when patients are assured that most people fully recover and when patients stay active and working as much as possible. Studies have shown it’s best to avoid prolonged inactivity and cervical collars unless under a doctor’s orders. It’s also a good idea to gradually introduce exercises aimed at improving range of motion, postural endurance, and motor control provided doing so keeps the patient within reasonable pain boundaries. Chiropractic manipulation restores movement in fixed or stuck joints in the back and neck and has been found to help significantly with neck pain and headaches, particularly for patients involved in motor vehicle collisions. A doctor of chiropractic may also recommend using a cervical pillow, home traction, massage, and other therapies as part of the recovery process.
It is important to be aware that fear of normal activity and not engaging in usual activities and work can delay healing and promote chronic problems and long-term disability. It’s suggested patients avoid opioid medication use due to the addictive problems with such drugs. Ice and anti-inflammatory herbs or nutrients (like ginger, turmeric, and bioflavonoids) are safer options. Your doctor of chiropractic can guide you in this process!
Why am I so dizzy after my whiplash?
Whiplash, or better termed “Whiplash Associated Disorders” (WAD), is a condition that carries multiple signs and symptoms ranging from neck pain and stiffness to headache, confusion, ringing in the ears, and more. But can WAD cause dizziness? Let’s take a look!
Dizziness is a general term that is used rather loosely by the general population. We’ve all experienced dizziness from time-to-time that is considered “normal,” such as standing up too quickly or while experiencing a rough flight.
Often, dizziness and problems with balance go hand in hand. There are three main organs that control our balance: 1) the vestibular system (the inner ear); 2) the cerebellum (lies in the back of the head); and, 3) the dorsal columns (located in the back part of the spinal cord). In this article, we will primarily focus on the inner ear because, of the three, it’s unique for causing dizziness. Our vision also plays an important role in maintaining balance, as we tend to lose our balance much faster when we close our eyes.
It’s appropriate to first discuss the transient, usually short episode of “normal” lightheadedness associated with rising quickly. This is typically caused by a momentary drop in blood pressure, and hence, oxygen simply doesn’t reach the brain quick enough when moving from sitting to standing. Again, this is normal and termed “orthostatic hypotension” (OH).
However, OH can be exaggerated by colds, the flu, allergy flair-ups, when hyperventilating, or at times of increased stress or anxiety. OH is also associated with the use of tobacco, alcohol, and/or some medications. Bleeding can represent a more serious cause of OH such as with bleeding ulcers or some types of colitis, and less seriously, with menstruation.
The term BPPV or benign paroxysmal positional vertigo, has to do with the inner ear where our semicircular canals are located. The canals lie in three planes and give us a 3D, 360º perspective about where we are in space. The fluid flowing through these canals bends little hair-like projections, which are connected to sensory nerves that tell the brain about our spatial position. If the function of these canals is disturbed, it can mix-up the messages the brain receives, thus resulting in dizziness. Exercises are available on the Internet that can help with BPPV (look for Epley’s and Brandt-Daroff exercises).
DANGEROUS causes of dizziness include: HEART – fainting (passing out) accompanied by chest pain, shortness of breath, nausea, pain or pressure in the back, neck, jaw, upper belly, or in one or both arms, sudden weakness, and/or a fast or irregular heartbeat.
STROKE – sudden numbness, paralysis, or weakness in the face, arm, or leg, especially if only on one side of the body; drooling, slurred speech, short “black outs,” sudden visual changes, confusion/difficulty speaking, and/or a sudden and severe, “out of the ordinary” headache. CALL 911 (or the number for emergency services if you’re outside the Canada) if you suspect you may be having a heart attack or stroke!
How can I calm down my WAD symptoms?

Whiplash is really a slang term for the rapid back and forth whipping of the head on the neck, usually associated with motor vehicle accidents. The title “Whiplash Associated Disorders”, or WAD, describes it best because it includes ALL of the MANY signs and symptoms of the disorder.
WAD basically comes in three sizes based on the degree of injury. A WAD I is present when there is pain but no physical examination findings; WAD II occurs when there are exam findings but no neurological loss (numbness or weakness); and WAD III includes loss of neurological function. There is also a separate WAD level that includes fractures and dislocations (WAD IV).
There are many things that can be done by the patient to assist in the healing process for WAD. The first well-studied recommendation is to “continue with your usual activities.” Try to keep active and not change your routine. The good news is that WAD (especially types I and II) usually resolves without complication, and recovery is even more likely to occur if you don’t deviate much from your routine.
For those whose symptoms are more severe and/or not resolving, mobilization and manipulation of the neck and back are very effective treatment options. In addition to treatments you’d receive in a chiropractic office, there are MANY things you can do at home as “self-help strategies.” Some of these include (“PRICE”):
1) PROTECT: Though it’s important to continue with your usual daily activities, this is dependent on both the degree of tissue injury and your pain tolerance. So do as many of your usual daily activities as possible, but AVOID those that result in a sharp, lancinating type of pain or those where recovery from the pain is delayed. Therefore, this category may require modifying your ADLs (activities of daily living). A cervical collar (hard orsoft) should NOT to be used UNLESS you have an unstable injury (fracture or a grade III sprain).
2) REST: Doing too much is like picking at a cut (which can delay healing) and doing too little can lead to a delayed healing response as well. Staying within reasonable pain boundaries is a good guide.
3) ICE > HEAT: Ice reduces swelling, and your doctor will typically recommend it over applying heat, especially on a recent injury. Heat draws fluids in, and while it may feel good, it can make your symptoms worse.
4) COMPRESS: We can basically ignore this when referencing neck pain. This pertains better to wrapping an ankle, knee, wrist, or elbow with an elastic compression orthotic or brace.
5) ELEVATE: This too is meant for the acute stages of an extremity injury like a foot or ankle.
Exercises unique for neck pain in the acute, subacute, and chronic stages of healing are perhaps the most important of the self-help approaches. In the ACUTE phase, try these…
1) Range of Motion: Once again, stay within “reasonable pain boundaries” as you move your head forwards, backwards, side to side, and rotate left and right. These can be done either with or without LIGHT resistance applied using one or two fingers placed against your head. Limit the repetitions to three slow reps in each direction and emphasize the release of the movement.
2) Chin/head Glides: Tuck in the chin (think of creating a double or triple chin) followed by poking the chin/head out.
In the SUBACUTE and CHRONIC phases of healing, the importance of strengthening the deep neck flexors cannot be over emphasized. Please refer to last week’s article for a description of this (see #3 of the 6 recommendations listed).
Entering & Exiting Your Vehicle

Entering and exiting your vehicle is a potential risky activity for low back pain sufferers. Follow these tips to limit problems:
✓ To enter the vehicle, open the door and stand with your back to the seat, legs close to the side of the vehicle. For larger vehicles, you may wish to begin by standing on the running board. Place your hands on the door and door frame to keep your movements slow and controlled then slowly lower your body into the vehicle.
✓ Tuck your head into the vehicle. Keep your knees close to each other, as though they have been taped together, brace your abdomen as though you are about to be punched in the stomach and pivot your body as a whole without twisting or bending at the waist. You may grasp the steering wheel with your right hand to help you pivot.
✓ Use a lumbar roll or other support to help maintain good posture. Position the roll slightly above your belt to support the “small of your back”. Adjust your seat so that your knees are slightly lower than your hips. Try to avoid prolonged car rides- take frequent breaks.
✓ Before exiting, create adequate space by pushing your vehicle seat back as far as possible and move the steering wheel up and out of the way. To exit, first scoot slightly to the door side edge of your seat, then keep your knees together and pivot with the same cautions that you used to enter the vehicle. When your feet are shoulder width apart and firmly on the ground or running board, grasp the door and door frame, lean forward, but be sure not to bend your back, as you tighten your abdominal muscles. Slowly thrust your hips forward to stand up.
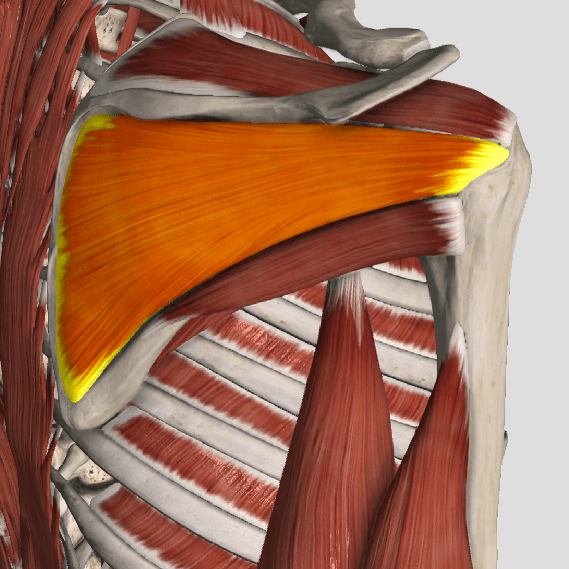
Trigger points in the trapezius muscle.
The trapezius muscle is a large diamond shaped muscle in you mid/upper back and neck. This muscle is one of the most common sites where trigger points can form. This muscle originates on the Nuchal ligament and the spinous processes of C6-T12. It inserts on the spine of the scapula, the acromion process, and the distal clavicle. The upper fibres elevate the shoulder and rotate the glenoid fossa (shoulder socket) upward. The lower fibres assist this motion as well as help depress the shoulder. The middle fibres of this muscle strongly adduct the scapula. This muscle is susceptible to postural overload such as sitting at desk all day. Trigger points on the lateral upper edge refer into the lateral neck and temples, causing “tension neck ache”as well as headache pain.Trigger points in the middle and lower fibres refer pain into the posterior neck and shoulder.