The trapezius muscle is a large diamond shaped muscle in your back and neck. It originates on the nuchal ligament and the spinous processes of c6-t12. It inserts on the scapular spine, acromion process, and the distal clavicle. It’s upper fibres act to elevate the shoulder and rotate the glenoid fossa upward. The lower fibres assist this motion. The middle fibres strongly adduct the scapula. This is the most common muscle in the human body to get trigger points. Trigger points in the lateral upper edge refer pain into the lateral neck and temples. Points in the mid and lower parts of the muscle refer pain into the posterior neck and shoulders. Trigger points in this muscle are a common cause of headaches.
Car Accident
Trigger point massage
Session Description
A treatment with Bryan is very user friendly. And, no, you don’t have to remove any clothing. However, bringing a t-shirt and a pair of shorts or sweats is recommended.
The first time you come for a treatment you will be asked to fill out a Client History form. Bryan will go over the information you provide, asking for more detail and discussing the type of pain you are having and its location.
The treatment itself involves locating the Trigger Points in the muscle or soft tissue and applying a deep focused pressure to the Point. This will reproduce the pain and the referral pattern that is characteristic of that pain.
The treatment will be uncomfortable at first, but as the Trigger Points release, the pain will decrease. The pressure will always be adjusted to your tolerance level. If, at any time, you feel too uncomfortable you can ask Bryan to ease off a bit.
Depending on your specific problem, Bryan may also use some stretching and / or range-of-motion techniques, as needed.
After treatment, it is usually recommended that the client apply moist heat to the area treate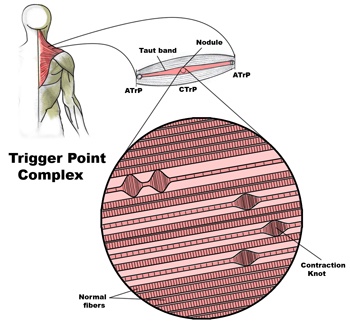
 d.
d.
Problems associated with trigger points
Trigger Points in muscle and other soft tissue are one of the most common causes of a wide variety of pain and dysfunction, including (but not limited to):
• Achy persistent pain
• Severe local pain
• Arm / leg pain
• Back pain
• Radiating pain
• Weakness
• Stiffness
• Pain resulting from a medical condition, such as
– Migraines
– Sciatica
– TMJ dysfunctions
– Arthritis
– Fibromyalgia
– Carpal tunnel syndrome
– Soft tissue injuries
– And more…
Trigger points in the levator scapula
The levator scapula is a muscle located in your neck. It originates on the transverse processes of C1-C4 vertebrae. It inserts on the superior part of the medial border of the scapula. This muscle acts to elevate the scapula and rotate the glenoid fossa downward. At the cervical attachment it acts to rotate the neck to the same side and assists extension. Trigger points will refer pain into the angle of the neck with spillover into the scapula. When this muscle is tight due to trigger points it will restrict neck rotation causing the classic stiff neck. With a forward head position this muscle often becomes stretched and over worked.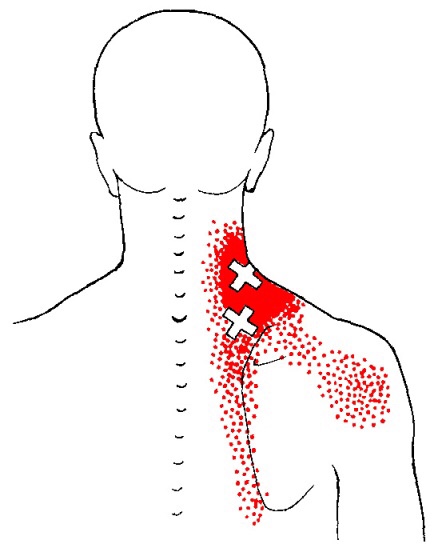
Trigger points in the lateral pterygoid muscle
The Lateral Pterygoid muscle is a muscle of the jaw. It originates on the greater wing of the sphenoid bone and the lateral pterygoid plate. It has its insertion on the condyloid process of the mandible. Functionally it it assists in opening the jaw by pulling the head of the mandibular condyle out of the mandibular fossa. Trigger points in this muscle refer pain into the temporal mandibular joint and maxillary sinus. Trigger points in this muscle are often the cause of pain felt from TMJ dysfunction.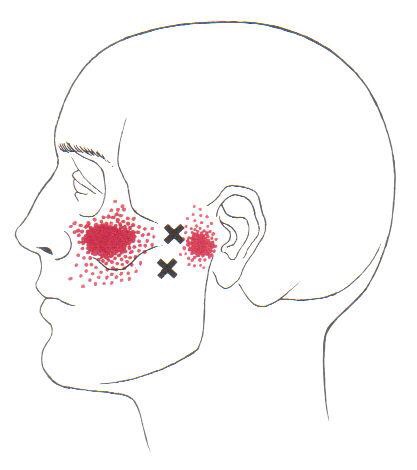
A treatment with Bryan Cobb RMT.
Session Description
A treatment with Bryan is very user friendly. And, no, you don’t have to remove any clothing. However, bringing a t-shirt and a pair of shorts or sweats is recommended.
The first time you come for a treatment you will be asked to fill out a Client History form. Bryan will go over the information you provide, asking for more detail and discussing the type of pain you are having and its location.
The treatment itself involves locating the Trigger Points in the muscle or soft tissue and applying a deep focused pressure to the Point. This will reproduce the pain and the referral pattern that is characteristic of that pain.
The treatment will be uncomfortable at first, but as the Trigger Points release, the pain will decrease. The pressure will always be adjusted to your tolerance level. If, at any time, you feel too uncomfortable you can ask Bryan to ease off a bit.
Depending on your specific problem, Bryan may also use some stretching and / or range-of-motion techniques, as needed.
After treatment, it is usually recommended that the client apply moist heat to the area treated.
What the Heck Is a Trigger Point?
By Bryan Cobb, Advanced Remedial Massage Therapist
What is a Trigger Point?
Trigger Points (TP’s) are defined as a “hyper-irritable spot within a taut band of skeletal muscle. The spot is painful on compression and can evoke characteristic referred pain and autonomic phenomena.”1
Put into plain language, a TP is a painful knot in muscle tissue that can refer pain to other areas of the body. You have probably felt the characteristic achy pain and stiffness that TP’s produce, at some time in your life.
TP’s were first brought to the attention of the medical world by Dr. Janet G. Travell. Dr. Travell, physician to President John F. Kennedy, is the acknowledged Mother of Myofascial Trigger Points. In fact, “Trigger Point massage, the most effective modality used by massage therapists for the relief of pain, is based almost entirely on Dr. Travell’s insights.”2 Dr. Travell’s partner in her research was Dr. David G. Simons, a research scientist and aerospace physician.
Trigger Points are very common. In fact, Travell and Simons state that TP’s are responsible for, or associated with, 75% of pain complaints or conditions.1 With this kind of prevalence, it’s no wonder that TP’s are often referred to as the “scourge of mankind”.
Trigger Points can produce a wide variety of pain complaints. Some of the most common are migraine headaches, back pain, and pain and tingling into the extremities. They are usually responsible for most cases of achy deep pain that is hard to localize.
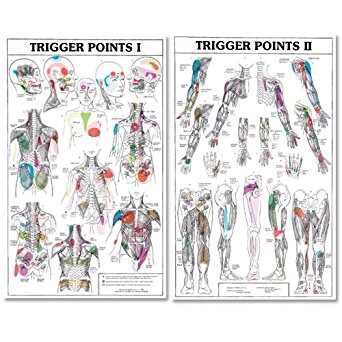
A TP will refer pain in a predictable pattern, based on its location in a given muscle. Also, since these spots are bundles of contracted muscle fibres, they can cause stiffness and a decreased range of motion. Chronic conditions with many TP’s can also cause general fatigue and malaise, as well as muscle weakness.
Trigger Points are remarkably easy to get, but the most common causes are
•
TP’s (black dots) can refer pain to other areas (red)

Sudden overload of a muscle
• Poor posture
• Chronic frozen posture (e.g., from a desk job), and
• Repetitive strain
Once in place, a TP can remain there for the remainder of your life unless an intervention takes place.
Trigger Points Not Well Known
With thousands of people dealing with chronic pain, and with TP’s being responsible for — or associated with — a high percentage of chronic pain, it is very disappointing to find that a large portion of doctors and other health care practitioners don’t know about TP’s and their symptoms.
Scientific research on TP’s dates back to the 1700’s. There are numerous medical texts and papers written on the subject.
But, it still has been largely overlooked by the health care field. This has led to needless frustration and suffering, as well as thousands of lost work hours and a poorer quality of life.
How Are Trigger Points Treated?
As nasty and troublesome as TP’s are, the treatment for them is surely straight-forward. A skilled practitioner will assess the individual’s pain complaint to determine the most likely location of the TP’s and then apply one of several therapeutic modalities, the most effective of which is a massage technique called “ischemic compression”.
Basically, the therapist will apply a firm, steady pressure to the TP, strong enough to reproduce the symptoms. The pressure will remain until the tissue softens and then the pressure will increase appropriately until the next barrier is felt. This pressure is continued until the referral pain has subsided and the TP is released. (Note: a full release of TP’s could take several sessions.)
Other effective modalities include dry needling (needle placed into the belly of the TP) or wet needling (injection into the TP). The use of moist heat and stretching prove effective, as well. The best practitioners for TP release are Massage Therapists, Physiotherapists, and Athletic Therapists. An educated individual can also apply ischemic compression to themselves, but should start out seeing one of the above therapists to become familiar with
the modality and how to apply pressure safely.
1 Simons, D.G., Travell, D.G., & Simons, L.S. Travell and Simons’ Myofascial Pain and Dysfunction: the Trigger Point Manual.
Vol. 1. 2nd ed. Lippincott, Williams, and Wilkins, 1999.
2http://www.muscletherapyworks.com/MTW%20Biography%20T%20&%20S%2001.htm
Trigger points in the deltoid muscle
The deltoid is the main muscle that makes up the shoulder. It originates on the clavicle, acromion, and spine of the scapula. It inserts on the deltoid tuberosity of the humerus. The deltoid acts at the shoulder to produce abduction, and assist with flexion and extension. The deltoid is especially prone to developing trigger points. These posterior style will refer pain into the anterior and lateral shoulder. Trigger points in the posterior delt will refer pain into the posterior shoulder with spillover down the lateral arm.
Lumbar Radiculopathy? That sounds ridiculous!
Your nervous system is basically a big electrical circuit. Your spinal cord transmits all of the electrical nerve impulses between your brain and lower back. From there, individual nerves emerge from your spine then travel to supply sensation and movement to a specific area of your buttock, legs and/or feet. This allows you to move and feel sensations like touch, heat, cold and pain. Anything that

interferes with this transmission can cause problems.
You have been diagnosed with a “Lumbar Radiculopathy”. This means that one or more of the nerves emerging from your lower back has become irritated or possibly pinched. This often results in pain, numbness or tingling in the specific area of your leg that is supplied by the irritated nerve. The term “Sciatica” is often used to describe this condition, because most (but not all) “lumbar radiculopathies” involve the sciatic nerve which supplies the back & outside of your thigh and calf. Symptoms of a lumbar radiculopathy may vary from a dull ache to a constant severe sharp shooting pain. Your symptoms are likely aggravated by certain positions or movements.
To solve this problem, we will treat the source of your nerve irritation. It is important for you to follow your treatment plan closely and be sure to tell us immediately if you experience any progression of your leg pain, numbness or weakness.
Lumbar Spondylolisthesis


the vertebral arches on its way from your brain to your tailbone. The term “lumbar isthmic spondylolisthesis” describes a condition where your arch has broken free from its anchor on the vertebral body, allowing the vertebral body to slide forward. Lumbar spondylolisthesis typically affects the lowest lumbar vertebra, L5, or occasionally the second lowest, L4.
The condition is sometimes caused by trauma, but more often follows a “stress fracture” involving the arch of the vertebra. This break and slippage is thought to result from repetitive movements, especially hyperextension (arching back) and rotation. The break usually happens during childhood but does not always cause symptoms when it occurs. Many times, the condition will lie dormant until later in life. Lumbar spondylolisthesis is present in six to seven percent of the population and affects males twice as often as females. The problem is more common in those who participate in sports. Some sports predispose children to this “break and slip”. Athletes who participate in gymnastics, rowing, diving, football, wrestling, weight lifting, swimming, tennis, volleyball, and track & field throwing sports (i.e. discus, shot put, etc) are at greatest risk.
The pain usually starts in your back but may radiate into your buttock or thigh. Your pain usually intensifies with standing upright for prolonged periods of time or leaning backwards, especially during heavy activity. Some women report increased symptoms during the later stages of pregnancy. Be sure to tell your doctor if you notice pain, numbness or tingling in your groin, a loss of bowel or bladder function, fever, night sweats, pain extending beyond your knee, or weakness in your legs.
Your doctor will “grade” your spondylolisthesis based on the percent of the vertebral body that has slipped forward. Your doctor will try to determine if your spondylolisthesis is “active”, meaning a recent break or “inactive”, referring to a long-standing problem. If your doctor has determined that your spondylolisthesis is new and has a chance of worsening, you may need to stop certain activities or sports for a period of time until your fracture heals. Sometimes a lumbar brace is used to help you recover more quickly. Patients with a long-standing “inactive” spondylolisthesis may benefit from a combination of treatments including stretching and strengthening. You should limit leaning backwards or sleeping on your stomach. Females should avoid wearing high heels.
Positive Expectations in Whiplash Patients Help with Recovery
“High expectations are the key to everything”
– Sam Walton
Now a new study found that this belief may apply to your health as well: Whiplash patients who have a positive expectation to improve tend to recover better and report less pain than those who harbor negative beliefs like fearing movement and re-injury.
If you or someone you know has been involved in accident, call our office today. Check out THIS VIDEO to learn more about resolving neck pain from auto accidents.
