The gluteus Maximus is the buttock muscle. It originates on the gluteal surface of the ilium, lumbar fascia, sacrum and sacrotuberous ligament. It inserts on the gluteal tuberosity of the femur and the iliotibial tract. Extension and lateral rotation of the hip are it’s main actions. This muscle is heavily involved in activities like ice skating and is a common area to develops trigger points. When trigger points do develop they can refer pain in a crescent pattern from the gluteal fold to the sacrum. Trigger points can also refer pain deep into the buttock itself making it feel like other deeper muscles are involved. These symptoms can sometimes be mistaken for s.i. Joint problems. 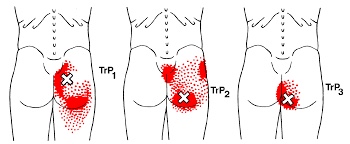
workout
Trigger points in the supraspinatus
The supraspinatus is a muscle of the rotator cuff. Is sits above the infraspinatus and originates on the supraspinous fossa of the scapula. It’s insertion point is the superior facet of the greater tubercle of the humerus. It’s main function is to abduct the arm at the glenohumeral joint working with the deltoid. All rotator cuff muscles act to secure and support the head of the humerus in the glenoid fossa during arm movements acting as a sling. This muscle often gets impinged during overhead movements such as painting a ceiling. When trigger points form in this muscle they primarily refer a deep achy pain into the mid deltoid area with spillover pain radiating down the arm into the elbow.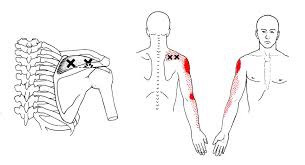
The Dreaded Lateral Ankle Sprain
“Ligaments” are made up of many individual fibers running parallel to each other and bundled to form a strong fibrous band. These fibrous bands hold your bones together. Just like a rope, when a ligament is stretched too far, it begins to fray or tear. “Sprain” is the term used to describe this tearing of ligament fibers.
Sprains are graded by the severity of damage to the ligament fibers. A Grade 1 sprain means the ligament has been painfully stretched, but no fibers have been torn. A Grade 2 sprain means some, but not all, of the ligaments’ fibers have been torn. A Grade 3 sprain means all of the ligaments’ fibers have been torn, and the ligament no longer has the ability to protect the joint.


Ankle sprains are the most common soft-tissue injury and will affect up to 20% of active people at some point in their life. Most ankle sprains occur because you have “rolled your ankle” inward. Sprains on the outer side of your ankle are much more common than sprains on the inner side. People who have suffered a prior ankle injury are more likely to suffer subsequent ankle injuries.
Ankle sprains cause pain and swelling over the outside of your ankle. Walking may be difficult, and bruising is common. Be sure to tell your doctor if you experience numbness, tingling, or a dramatic cold sensation in your foot, as this may indicate more significant injury.
Ankle sprains can be successfully managed but will require some work on your part. You can help reduce swelling by elevating your ankle by lying or sitting with your foot elevated or by using an ACE wrap for compression. Applying ice or ice massage for 10 minutes each hour may help relieve swelling. Depending upon the severity of your sprain, you may need to wear an ankle brace to help protect you from further injury. If walking is painful, crutches may be necessary.
Initially, a period of rest may be necessary in order to help you heal. Mild Grade 1 sprains may allow return to sport in a couple of days, while more severe injuries may take six weeks or longer to recover. Surgery is rarely necessary.
Trigger points in the infraspinatus
The infraspinatus muscle is one of the muscles that makes up the rotator cuff. It originates on the infraspinous fossa of the scapula, and inserts on the middle facet of the greater tubercle of the humerus. It functions to externally rotate the humerus and to stabilize the head of the humerus in the glenoid cavity during upward movement of the arm. Trigger points in this muscle refer pain deep into the anterior shoulder joint and down the anterior arm. Trigger points near the lower medial border refer pain into the rhomboids. This muscle is often injured during throwing motions.
Is there an actual cure all?
No; but exercise seems to be as close as we will ever get!
Some of you may have heard about how a modified form of boxing is helping patients with Parkinson’s disease (PD). If you haven’t, it’s been observed that people with Parkinson’s disease (PD) who engage in this boxing-like exercise routine can enhance their quality of life and even build impressive gains in posture, strength, flexibility, and speed. Proponents of the program report that regardless the degree of severity of PD, participants have a happier, healthier, and higher quality of life.
But must it be boxing? Maybe not. A report presented at the International Congress of Parkinson’s Disease and Movement Disorders in San Diego in June 2015 found that patients with Parkinson’s disease who began regular exercise early into the PD process had a much slower decline in their quality of life when compared with those who started exercising later. The researchers found just 2.5 hours per week of exercise is needed to improve quality of life scores. According to the report, it didn’t matter what exercise the participants did — simply getting up and moving for a total of 2.5 hours/week was reportedly enough (that’s only 20-25 minutes / day)!
Looking beyond Parkinson’s, other chronic conditions also benefit from adding exercise into a person’s lifestyle. Studies show that regular exercise as simple as walking helps reduce one’s risk for memory loss, and it slows down functional decline in the elderly. Incorporating aerobic exercise into one’s lifestyle can also improve reaction time in people at ALL AGES. Exercise has also been shown to improve both physical and emotional well-being in those afflicted with Alzheimer’s disease with as little as 60 minutes/week of moderate exercise! Patients with multiple sclerosis (MS) have also reported less stiffness and less muscle wasting when using exercise machines, aquatic exercise, and/or walking.
Research has shown just 30 minutes of brisk exercise three times a week can help reduce depressive symptoms in patients with mild-to-moderate depression. In a study involving teenagers, those who engaged in sports reported a greater level of well-being than their sedentary peers, and the more vigorous the exercise, the better their emotion health! In kids 8-12 years old, physical inactivity is strongly linked to depression.
Even anxiety, stress, and depression associated with menopause are less severe in those who exercise! So LET’S ALL GET OUT THERE AND EXERCISE!!!
Exercise Tip Of The Month

Women are often afraid to lift weights for fear they will look too “bulky”, but actually
that’s not what happens.
Women can and should do weight lifting exercises if they want to shed body fat and achieve a toned physique. Strength training 30 to 40 minutes twice a week for 4 months, could increase an average woman’s resting metabolism by 100 calories a day, meaning you’ll be burning calories even when you’re not exercising.
Trigger points in the triceps muscle.
The tricep muscle is named for its three heads long, medial, and lateral. The long head originates on the infraglenoid tubercle, the medial head on the posterior humerus, and the lateral head on the posterior humerus as well. They join together to insert on the Olecranon process of the ulna. The triceps function to extend the elbow. Strong extension under resistance can cause trigger points to form. Pain referred from triceps trigger points can be felt in the posterior shoulder and down the posterior forearm, as well as in in the olecranon process and the lateral epicondyle which can cause “tennis elbow” pain.
My knee hurts; I must have bad knees….
Due to bipedal locomotion (walking around on two legs), foot and ankle problems have the potential to affect EVERYTHING above the feet—even the knees!
When analyzing the way we walk (also known as our gait), we find when the heel strike takes place, the heel and foot motion causes “supination” or the rolling OUT of the ankle. As the unloaded leg begins to swing forwards, there is a quick transition to pronation where the heel and ankle roll inwards and the medial longitudinal arch (MLA) of the foot flattens and pronates NORMALLY!
During the transition from supination to pronation, the flattening of the MLA acts like a spring to propel us forwards followed by the “toe off”, the last phase, as we push off with our big toe and the cycle starts with the other leg. However, if you watch people walk from behind, you will see MANY ankles roll inwards too much. This is call “hyperpronation” and that is NOT NORMAL!
So at what point does this normal pronation become hyperpronation? The answer is NOT black and white, as there is no specific “cut-off” point but rather, a range of abnormal. Hence, we use the terms mild, moderate, and severe hyperpronation to describe the variance or the degrees of abnormality. Hyperpronation can lead to the development of bunions and foot/ankle instability that can cause and/or contribute to knee, hip, pelvis, and spinal problems—even neck and head complaints can result (the “domino effect”)!
One study looked at the incidence of hyperpronation in 50 subjects who had an anterior cruciate ligament (ACL) rupture vs. 50 without a history of knee / ACL injury. They found the ACL-injured subjects had greater pronation than the noninjured subjects suggesting that the presence of hyperpronation increases the risk of ACL injury.
Doctors of chiropractic are trained to evaluate and treat knee conditions of all kinds. Often this may include prescribing exercises or utilizing foot orthotics in an effort to restore the biomechanics of the foot, which can have positive effects not only on the knees but also further up the body.
Pathophysiology of trigger points.
A large number of factors have been identified as causes of trigger point activation. These include acute or chronic overload of muscle tissue, disease, psychological distress, systemic inflammation, homeostatic imbalances, direct trauma, radiculopathy, infections, and lifestyle choices such as smoking. Trigger points form as a local contraction of muscle fibres in a muscle or bundle of muscle fibres. These can pull on ligaments and tendons associated with the muscle which can cause pain to be felt deep inside a joint. It is theorized that trigger points form from excessive release of acetylcholine causing sustained depolarization of muscle fibres. Trigger points present an abnormal biochemical composition with elevated levels of acetylcholine, noradrenaline and serotonin and a lower ph. The contracted fibres in a trigger point constricts blood supply to the area creating an energy crisis in the tissue that results in the production of sensitizing substances that interact with pain receptors producing pain. When trigger points are present in a muscle there is often pain and weakness in the associated structures. These pain patterns follow specific nerve pathways that have been well mapped to allow for accurate diagnosis or the causative pain factor.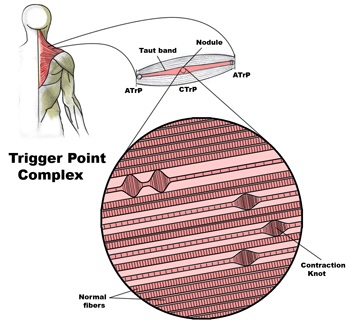
Diagnosis of trigger points.
Diagnosis of trigger points typically takes into account symptoms, pain patterns, and manual palpation. When palpating the therapist will feel for a taut band of muscle with a hard nodule within it. Often a local twitch response will be elicited by running a finger perpendicular to the muscle fibres direction. Pressure applied to the trigger point will often reproduce the pain complaint of the patient and the referral pattern of the trigger point. Often there is a heat differential in the local area of the trigger point. 


