The levator scapula is a muscle located in your neck. It originates on the transverse processes of C1-C4 vertebrae. It inserts on the superior part of the medial border of the scapula. This muscle acts to elevate the scapula and rotate the glenoid fossa downward. At the cervical attachment it acts to rotate the neck to the same side and assists extension. Trigger points will refer pain into the angle of the neck with spillover into the scapula. When this muscle is tight due to trigger points it will restrict neck rotation causing the classic stiff neck. With a forward head position this muscle often becomes stretched and over worked.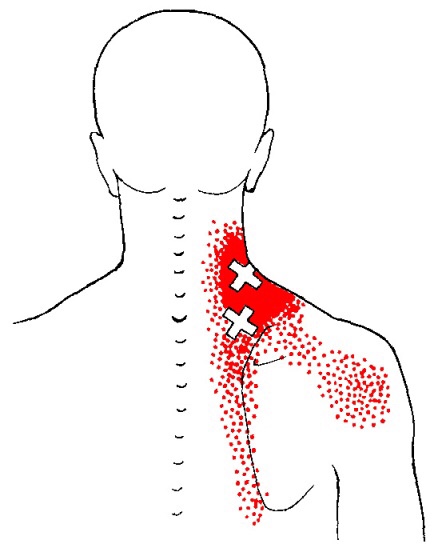
Whiplash
A treatment with Bryan Cobb RMT.
Session Description
A treatment with Bryan is very user friendly. And, no, you don’t have to remove any clothing. However, bringing a t-shirt and a pair of shorts or sweats is recommended.
The first time you come for a treatment you will be asked to fill out a Client History form. Bryan will go over the information you provide, asking for more detail and discussing the type of pain you are having and its location.
The treatment itself involves locating the Trigger Points in the muscle or soft tissue and applying a deep focused pressure to the Point. This will reproduce the pain and the referral pattern that is characteristic of that pain.
The treatment will be uncomfortable at first, but as the Trigger Points release, the pain will decrease. The pressure will always be adjusted to your tolerance level. If, at any time, you feel too uncomfortable you can ask Bryan to ease off a bit.
Depending on your specific problem, Bryan may also use some stretching and / or range-of-motion techniques, as needed.
After treatment, it is usually recommended that the client apply moist heat to the area treated.
What the Heck Is a Trigger Point?
By Bryan Cobb, Advanced Remedial Massage Therapist
What is a Trigger Point?
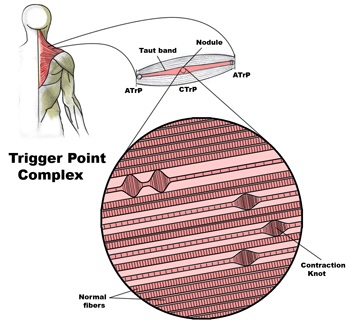
Trigger Points (TP’s) are defined as a “hyper-irritable spot within a taut band of skeletal muscle. The spot is painful on compression and can evoke characteristic referred pain and autonomic phenomena.”1
Put into plain language, a TP is a painful knot in muscle tissue that can refer pain to other areas of the body. You have probably felt the characteristic achy pain and stiffness that TP’s produce, at some time in your life.
TP’s were first brought to the attention of the medical world by Dr. Janet G. Travell. Dr. Travell, physician to President John F. Kennedy, is the acknowledged Mother of Myofascial Trigger Points. In fact, “Trigger Point massage, the most effective modality used by massage therapists for the relief of pain, is based almost entirely on Dr. Travell’s insights.”2 Dr. Travell’s partner in her research was Dr. David G. Simons, a research scientist and aerospace physician.
Trigger Points are very common. In fact, Travell and Simons state that TP’s are responsible for, or associated with, 75% of pain complaints or conditions.1 With this kind of prevalence, it’s no wonder that TP’s are often referred to as the “scourge of mankind”.
Trigger Points can produce a wide variety of pain complaints. Some of the most common are migraine headaches, back pain, and pain and tingling into the extremities. They are usually responsible for most cases of achy deep pain that is hard to localize.
A TP will refer pain in a predictable pattern, based on its location in a given muscle. Also, since these spots are bundles of contracted muscle fibres, they can cause stiffness and a decreased range of motion. Chronic conditions with many TP’s can also cause general fatigue and malaise, as well as muscle weakness.
Trigger Points are remarkably easy to get, but the most common causes are
•
TP’s (black dots) can refer pain to other areas (red)

Sudden overload of a muscle
• Poor posture
• Chronic frozen posture (e.g., from a desk job), and
• Repetitive strain
Once in place, a TP can remain there for the remainder of your life unless an intervention takes place.
Trigger Points Not Well Known
With thousands of people dealing with chronic pain, and with TP’s being responsible for — or associated with — a high percentage of chronic pain, it is very disappointing to find that a large portion of doctors and other health care practitioners don’t know about TP’s and their symptoms.
Scientific research on TP’s dates back to the 1700’s. There are numerous medical texts and papers written on the subject.
But, it still has been largely overlooked by the health care field. This has led to needless frustration and suffering, as well as thousands of lost work hours and a poorer quality of life.
How Are Trigger Points Treated?
As nasty and troublesome as TP’s are, the treatment for them is surely straight-forward. A skilled practitioner will assess the individual’s pain complaint to determine the most likely location of the TP’s and then apply one of several therapeutic modalities, the most effective of which is a massage technique called “ischemic compression”.
Basically, the therapist will apply a firm, steady pressure to the TP, strong enough to reproduce the symptoms. The pressure will remain until the tissue softens and then the pressure will increase appropriately until the next barrier is felt. This pressure is continued until the referral pain has subsided and the TP is released. (Note: a full release of TP’s could take several sessions.)
Other effective modalities include dry needling (needle placed into the belly of the TP) or wet needling (injection into the TP). The use of moist heat and stretching prove effective, as well. The best practitioners for TP release are Massage Therapists, Physiotherapists, and Athletic Therapists. An educated individual can also apply ischemic compression to themselves, but should start out seeing one of the above therapists to become familiar with
the modality and how to apply pressure safely.
1 Simons, D.G., Travell, D.G., & Simons, L.S. Travell and Simons’ Myofascial Pain and Dysfunction: the Trigger Point Manual.
Vol. 1. 2nd ed. Lippincott, Williams, and Wilkins, 1999.
2http://www.muscletherapyworks.com/MTW%20Biography%20T%20&%20S%2001.htm
TMJ dysfunction
Temporomandibular joint dysfunction is a blanket term that refers to pain and dysfunction of the jaw muscles and the tempomandibular joints which connect the mandible to the skull. The most common symptoms are pain and restricted mandibular movement as well as grinding noises coming from the joint. This condition is more common in women then in men, and affects a large portion of patients suffering from fibromyalgia. Trigger points in the muscles of mastication are frequently involved in TMJ dysfunction. Trigger points in the pterygoid and masseter muscles for example will not only refer pain into the tempomandibular joints, but will also cause a dysfunctional movement pattern that can restrict range of motion. Trigger point therapy can be an effective modality to treat TMJ dysfunction.

Trigger points and fibromyalgia
Myofascial pain syndrome (trigger points) and fibromyalgia are often confused to be the same condition and while there is a lot of interrelatedness between the two they are not quite identical. The clinical definition of a trigger point is “a hyper irritable spot associated within a taut band of skeletal muscle that is painful on compression or muscle contraction, and usually responds with a referred pain pattern distant from the spot”. Trigger points form from an overload trauma to the muscle tissue. This is contrasted with fibromyalgia which is defined as “a medical condition characterized by chronic widespread pain and a heightened pain response to pressure. Other symptoms include tiredness to a degree that normal activities are affected, sleep problems and troubles with memory. Some people also report restless leg syndrome, bowel and bladder problems, numbness and tingling and sensitivity to noise, lights and temperature. It is also associated with depression, anxiety, and post traumatic stress disorder”. Fibromyalgia will also present with localized tender points which are often mistaken for trigger points. Where these two conditions become somewhat interrelated is via the nervous system. Fibromyalgia patients suffer from a super-sensitization of the nervous system causing hyperirritability and pain. Myofascial trigger points can be caused by,or be the cause of, super sensitization. An active trigger point will irritate the sensory nerves around it eventually leading to super-sensitization. Trigger points have also been showed to form of become active due to super-sensitization. Both of these conditions can perpetuate the other, leading to layers of pain and symptoms. This being the case, trigger point therapy can have a very positive effect on decreasing the severity of pain and symptoms in patients suffering from fibromyalgia.

Bryan Cobb RMT.
Since 2005, Bryan has been dedicated to helping all people with chronic and acute pain caused by soft-tissue damage.
His training and experience make him uniquely qualified to treat a wide variety of pain and dysfunction and to give instruction on prevention and self-care.
Bryan is the only Massage Therapist in Manitoba — and one of the few in Canada — to be certified by the Certification Board for Myofascial Trigger Point Therapists (CBMTPT).
Bryan holds a degree as an Advanced Remedial Massage Therapist (ARMT) from the Massage Therapy College of Manitoba. Course work at MTCM includes
• over 2,000 hours of practice, as well as
• intensive course work,
• a supervised clinical practicum, and
• community outreach placements.MTCM has a credit transfer affiliation with the University of Winnipeg, ensuring that its courses are held to the highest level. When Bryan studied at MTCM, the college was the only massage therapy college in western Canada accredited by the Commission on Massage Therapy Accreditation. Today, the college is a member of the Canadian Council of Massage Therapy Schools.
Bryan is a member in good standing of the Natural Health Practitioners of Canada.
Bryan also has a background in Anatomy, Exercise Physiology, and Sport Sciences from the University of Manitoba, and he has worked as a personal trainer and fitness leader.
He is an avid natural bodybuilder and fitness enthusiast, and has a blue belt in Brazilian jiu-jitsu.
Do you wake up with numb fingers?
The term “thoracic outlet” describes an area at the base of your neck, just above your collarbone. Some important nerves and vessels pass through this outlet on their way into your arm. Compression of these tissues causes a condition called “thoracic outlet syndrome” which results in pain, numbness or tingling in your arm.
Several different factors can cause Thoracic Outlet Syndrome,

commonly referred to as TOS. Sometimes TOS is caused from tightness in the muscles of your neck and chest, other times the space between your first rib and collarbone is too small. People who have an extra rib (cervical rib) and people who have recently suffered a neck injury may have a greater chance of having this problem.
The condition is aggravated by poor posture and by occupations that promote “slouching,” i.e., computer users, assembly line workers, supermarket checkers and students. Swimmers, volleyball players, tennis players, baseball pitchers and occupations requiring prolonged overhead activity. i.e., electricians and painters are also prime candidates for TOS.
Symptoms of TOS include arm pain, numbness, tingling and possible weakness. Neck, arm and hand pain may begin slowly and are often aggravated by elevation of the arms or excessive head movement. Loss of grip strength is possible.
Conservative treatment, like the kind we provide, has been shown to be effective at treating TOS. Through our careful exam we have identified your specific sites of compression and will use some of the following treatment to help:
You should avoid carrying heavy loads, especially on your shoulder i.e., carpet rolls. Briefcases, laptop cases or heavy shoulder bags should be lightened. Bra straps may need additional padding or consideration of replacement with a sports bra.
Trigger points in the lateral pterygoid
The lateral pterygoid muscle plays an important role in prober jaw function. It originates on the greater wing of the sphenoid bone and the lateral pterygoid plate, and inserts on the condyloid process of the mandible. It’s action is to pull the head of the mandibular condyle out of the mandibular fossa while opening the jaw. When trigger points develop they refer pain into the temporal mandibular joint and maxillary sinus. This referral is commonly mistaken for TM arthritis. In addition to the referral pain, trigger points in this muscle can also effect proper movement of the jaw.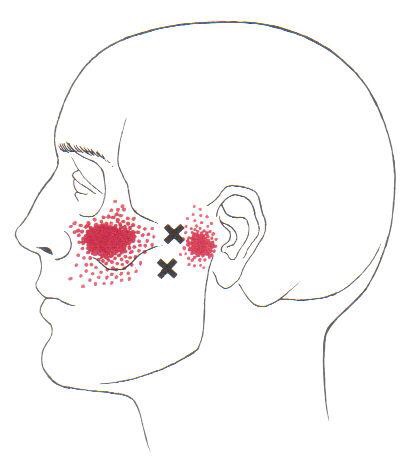

Can Chiro help me?

Chiropractic is the most widely accepted and most frequently used type of “alternative” healthcare in the United States. This is largely due to the fact that it works, and because of that, there has been a steady increase in acceptance by the public, third-party payers, and the Federal government. Since the mid-1990s, a number of outside (non-chiropractic) observers have suggested that chiropractic has now entered mainstream healthcare.
One can position chiropractic as being BOTH alternative and mainstream. It is “alternative” since it approaches healthcare from an entirely different direction compared to the primary care medical profession. Chiropractic is non-surgical and promotes diet and nutritional approaches vs. drugs and surgery. Chiropractic is also arguably “mainstream” as it has evolved into a strongly utilized form of primary care through popular acceptance and utilization by the public.
So, what role does chiropractic play in today’s health delivery system? This question is still being debated, but there appears to be three camps: 1) Specialist—limited to musculoskeletal (MSK) complaints on an interdisciplinary primary healthcare team; 2) Primary healthcare “gatekeepers” that focus on ambulatory MSK complaints; 3) Generalist primary healthcare provider of “alternative or complementary” medicine that manage and/or co-manage both MSK AND non-MSK conditions.
Looking at this from the patient or “consumer” perspective, chiropractic already plays an important role in the healthcare delivery for many patients. In 1993, a report claimed 7% of American adults had received chiropractic care during the prior year. According to a 2015 Gallup poll (that included 5,442 adults, aged 18+, surveyed between 2/16/15 and 5/6/15) entitled, Majority in U.S. Say Chiropractic Works for Neck, Back Pain, “Chiropractic care has a positive reputation among many US adults for effective treatment of neck and back pain, with about six in 10 adults either strongly agreeing (23%) or agreeing somewhat (38%) that chiropractors are effective at treating these types of pain.”
The “highlights” from this Gallup poll include: 1) Two-thirds say chiropractic is effective for neck and back pain. 2) Many adults say chiropractors think of the patient’s best interest. 3) More than 33 million adults in the United States (US) saw a chiropractor in the twelve months before the survey was conducted. That means roughly 14% of U.S. adults saw a chiropractor in the 12 months prior to the survey (vs. 7% in 1993). An additional 12% who responded to the Gallup pollsters saw a chiropractor in the last five years but not in the last 12 months. Overall, 51% of those polled had previously seen a chiropractor.
Whether or not you have personally utilized chiropractic, the educational process, licensing requirements, public interest, third-party payer systems, and interprofessional cooperation ALL support firm ground for which you can comfortably and confidently seek chiropractic care for your complaints.
We realize you have a choice in whom you consider for your health care provision and we sincerely appreciate your trust in choosing our service for those needs. If you, a friend, or family member requires care, we would be honored to render our services.
Work Station Ergonomics Advice
When dealing with Upper Crossed Syndrome the ergonomics of your workstation should be at the from of mind. Some workstation ergonomics advice is as follows:
Pathophysiology of trigger points.
A large number of factors have been identified as causes of trigger point activation. These include acute or chronic overload of muscle tissue, disease, psychological distress, systemic inflammation, homeostatic imbalances, direct trauma, radiculopathy, infections, and lifestyle choices such as smoking. Trigger points form as a local contraction of muscle fibres in a muscle or bundle of muscle fibres. These can pull on ligaments and tendons associated with the muscle which can cause pain to be felt deep inside a joint. It is theorized that trigger points form from excessive release of acetylcholine causing sustained depolarization of muscle fibres. Trigger points present an abnormal biochemical composition with elevated levels of acetylcholine, noradrenaline and serotonin and a lower ph. The contracted fibres in a trigger point constricts blood supply to the area creating an energy crisis in the tissue that results in the production of sensitizing substances that interact with pain receptors producing pain. When trigger points are present in a muscle there is often pain and weakness in the associated structures. These pain patterns follow specific nerve pathways that have been well mapped to allow for accurate diagnosis or the causative pain factor.