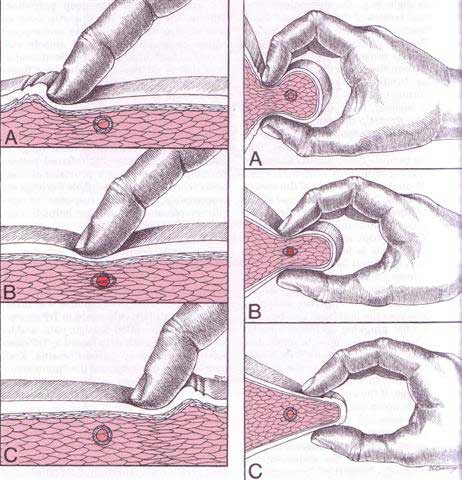
Diagnosis of trigger points typically takes into account symptoms, pain patterns, and manual palpation. When palpating the therapist will feel for a taut band of muscle with a hard nodule within it. Often a local twitch response will be elicited by running a finger perpendicular to the muscle fibres direction. Pressure applied to the trigger point will often reproduce the pain complaint of the patient and the referral pattern of the trigger point. Often there is a heat differential in the local area of the trigger point. 
Shoulder Pain
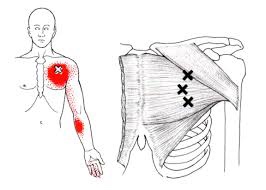
Trigger points in the biceps Brachii muscle.
The Bicep Brachii is perhaps the most recognizable muscle in the body. It’s the muscle that is most often flexed when someone says ” show me your muscles”. It is composed of two heads, the long head and the short head. The short head originates on the coracoid process of the scapula, and the long head on the supraglenoid tubercle. Both heads merge to insert on the radial tuberosity and bicipital aponeurosis into the deep fascia on the medial part of the forearm. The main actions of this muscle are elbow flexion and forearm supination(rotation with the palm of the hand going upward). This muscle also assists shoulder flexion. Trigger points in this muscle mainly refer pain into the shoulder, with spillover into the posterior aspect above the scapula. A less common referral is into the anterior elbow and forearm. 
What is a trigger point
Dr Janet travel coined the term trigger point in 1942 to describe clinical findings with characteristics of pain related a discrete irritable point in muscle or fascia that was not caused by acute trauma, inflammation, degeneration, neoplasm or infection. The painful point can be palpated as a nodule or tight band in the muscle that can produce a local twitch response when stimulated. Palpation of the trigger point reproduces the pain and symptoms of the patient and the pain radiates in a predictable referral pattern specific to the muscle harbouring the trigger point.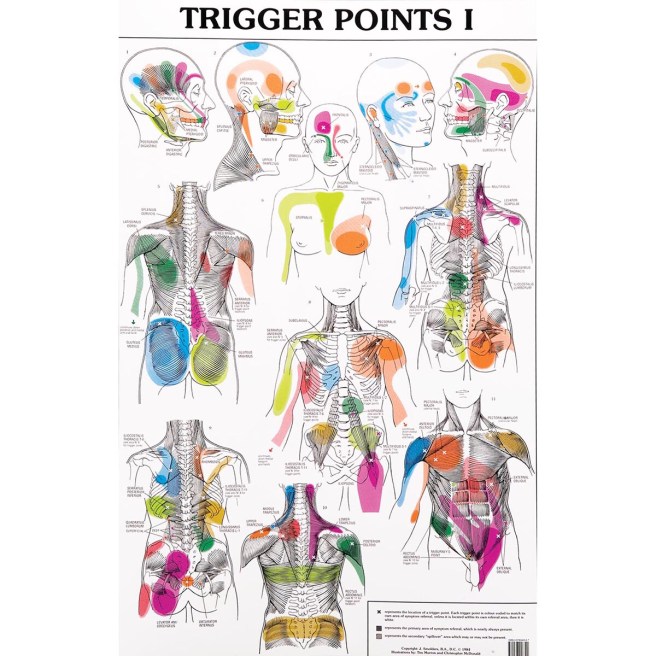
What to expect with a trigger point massage.
A treatment with Bryan is very user friendly. And, no, you don’t have to remove any clothing. However, bringing a t-shirt and a pair of shorts or sweats is recommended.
The first time you come for a treatment you will be asked to fill out a Client History form. Bryan will go over the information you provide, asking for more detail and discussing the type of pain you are having and its location.
The treatment itself involves locating the Trigger Points in the muscle or soft tissue and applying a deep focused pressure to the Point. This will reproduce the pain and the referral pattern that is characteristic of that pain.
The treatment will be uncomfortable at first, but as the Trigger Points release, the pain will decrease. The pressure will always be adjusted to your tolerance level. If, at any time, you feel too uncomfortable you can ask Bryan to ease off a bit.
Depending on your specific problem, Bryan may also use some stretching and / or range-of-motion techniques, as needed.
After treatment, it is usually recommended that the client apply moist heat to the area treated.
Trigger points in the deltoid muscle.
The deltoid is the the muscle that is most often thought of as the “shoulder.” It is the diamond shaped muscle that caps the shoulder joint. It originates on the clavicle, the acromion, and the spine of the scapula. It inserts on the deltoid tuberosity of the humerus. As a whole unit the deltoid laterally abducts the humerus at the glenohumeral joint. The anterior portion of the delt forward flexes the arm, as well as horizontally flexing the arm across the chest. Since the deltoid is involved in almost all shoulder movements it is especially prone to trigger points. Points in the anterior deltoid refer into the anterior and lateral shoulder. Trigger points in the posterior deltoid refer pain into the posterior shoulder with spillover down the lateral arm. 
Trigger points in the pectoralis minor muscle.
The pectoralis minor is a small strap like muscle that is underneath (deep) to the pectoralis major. It originates on the third to fifth rib, near the costal cartilages. It’s insertion is on the coracoid process of the scapula. It acts to draw the scapula forward, downward, and inward at nearly equal angles ( think of rounding or shrugging your shoulders forward). This muscle is very often shortened and tight in people due to the high prevalence of desk jobs. This muscle pulls the shoulder blade forward resulting in the muscles in the back(rhomboid and mid traps) being chronically strained. Trigger points that form in the pec minor primarily refer pain over the anterior chest and shoulder, with spillover down the medial arm. Trigger points in the left side can mimic angina. 
Trigger points in the pectoralis Major muscle.
The pectoralis major or “pecs” is commonly thought of as the chest muscle. It originates on the clavicle, sternum, costal cartilage , and the external oblique aponeurosis. It inserts on the intertubercular groove of the humerus. Its main actions are to adduct the shoulder and to internally rotate the humerus. This muscle gets chronically shortened by a rounded shoulder forward posture such as from prolonged sitting. Tightness in this muscle can cause strain in the rhomboids and traps. When trigger points form in this muscle they refer pain into the anterior shoulder, as well as the anterior chest and medial aspect of the arm. Trigger points in the pecs can also cause nipple hypersensitivity. Trigger points in the left pec muscle can mimic heart pain.
Trigger points in the trapezius muscle.
The trapezius muscle is a large diamond shaped muscle in you mid/upper back and neck. This muscle is one of the most common sites where trigger points can form. This muscle originates on the Nuchal ligament and the spinous processes of C6-T12. It inserts on the spine of the scapula, the acromion process, and the distal clavicle. The upper fibres elevate the shoulder and rotate the glenoid fossa (shoulder socket) upward. The lower fibres assist this motion as well as help depress the shoulder. The middle fibres of this muscle strongly adduct the scapula. This muscle is susceptible to postural overload such as sitting at desk all day. Trigger points on the lateral upper edge refer into the lateral neck and temples, causing “tension neck ache”as well as headache pain.Trigger points in the middle and lower fibres refer pain into the posterior neck and shoulder. 
Chiropractic as THE alternative to Opioids.
In 2015, two million Americans had a substance abuse disorder involving prescription pain relievers; with more than 20,000 overdose deaths related to these drugs. In the past decade, death rates and substance use rates quadrupled in parallel to sales of prescription pain relievers.
Chronic LBP is a primary generator for opioid prescriptions. This year, both JAMA and Annals of Internal Medicine have published and supported new clinical practice guidelines that recommend prescribing spinal manipulation over medication for LBP patients.
“For acute, subacute, or chronic low back pain, physicians and patients initially utilize spinal manipulation and delay pharmacologic management.”
Research shows that low back pain patients who undergo chiropractic care have improved outcomes with lower rates of opioid use, surgery, and overall healthcare costs.
Not surprisingly, various governing bodies, including the FDA, CDC, and 37 State Attorney General’s, have concurred that physicians and healthcare decision makers should consider non- pharmacologic therapy for LBP patients. In fact, the 2018 Joint Commission guidelines mandate that hospitals include conservative options for chronic musculoskeletal pain management, specifically naming chiropractic as a potential option.
Chiropractic care is not a replacement for traditional medical treatment of LBP, rather a complementary tool to integrate within your current management paradigm. We hope that you will continue to consider our office for those cases that may be favorably served by conservative manual therapy. We are grateful for your confidence and will work hard to maintain your trust.
