Your Achilles tendon is the strong fibrous band of tissue that connects your calf muscles to your heel. The tendon is named after “Achilles” who was a powerful, yet vulnerable warrior in Greek mythology. Likewise, our Achilles tendon, being the largest and strongest tendon in the body, is susceptible to injury from the high demands placed on it. (Running can generate forces over 12 times your bo
dy weight on the Achilles tendon.)
The tendon may be strained or even ruptured from excessive stretch or forceful contraction of the calf muscles. More commonly, the tendon is repeatedly overloaded and suffers tiny “micro tears.” Damage usually occurs either directly behind the heel, or near the weakest area of the tendon- one to two inches above the heel.
Achilles tendon injuries affect between 250,000 and 1 million people per year. Most are middle-aged males, between the age of 30 and 50. Interestingly, Achilles tendon injuries occur more frequently on the left side. If you have suffered a prior Achilles tendon injury, you are at greater risk of injuring the opposite side. Two-thirds of all Achilles tendon injuries involve athletes. Runners are up to 10 times more likely to suffer Achilles tendon problems. You may at increased risk if the arch of your foot is too high or too flat.
Symptoms may begin abruptly following a strain but more commonly develop slowly from repeated irritation. Morning pain and stiffness are common. Your symptoms will likely increase with activity, especially walking or running. You may notice pain when you rise up on your toes. Walking down stairs stretches the tendon and usually increases symptoms. Some patients notice that the irritated area becomes firmly swollen. Ongoing irritation to the spot on your heel where the tendon inserts can cause a painfully elevated “pump bump.”
Research has shown that conservative care, like the type provided in this office, can produce “excellent results” in over 85% of patients. Initially, you may need to limit or stop activities that cause pain. Runners may need to switch to swimming or cycling for a short period of time. Be sure to introduce new activities slowly and avoid increasing your activity by more than 10% per week. Runners should begin on a smooth, shock-absorbent surface and start at a low intensity – first increasing distance, then pace. Avoid training on hard or unlevel surfaces like hills. Make sure you warm up properly and avoid over training. Avoid wearing high heels or shoes with an excessively rigid heel tab. One of the most important and effective treatments for Achilles tendinopathy is performing “heel drop exercises” as outlined below.
Eccentric Achilles Strengthening
Begin standing up on your toes with the affected foot on the edge of a step. Do not place weight on your good leg, but you may use it for stability. Slowly lower your affected heel, at a count of 4 seconds, until you reach a fully stretched position and can drop no further. Use your good leg to return to your toes. Repeat 3 sets of 15 repetitions with your knee straight and 3 more sets of 15 repetitions with your knee slightly bent, twice daily or as directed. Moderate pain during this exercise is acceptable but if pain is excessive, you should assist downward motion with the non-injured leg.
Here is a brief description of the treatments we may use to help manage your problem.
Joint Manipulation
Your chiropractor has found joints in your body that are not moving freely. This can cause tightness and discomfort and can accelerate unwanted degeneration i.e. arthritis. Your chiropractor will apply a gentle force with their hands, or with hand held instruments, in order to restore motion to any “restricted” joints. Sometimes a specialized table will be used to assist with these safe and effective “adjustments”. Joint manipulation improves flexibility, relieves pain and helps maintain healthy joints.
Therapy Modalities
We may apply electrotherapy modalities that produce light electrical pulses transmitted through electrodes placed over your specific sites of concern. These comfortable modalities work to decrease your pain, limit inflammation and ease muscle spasm. Hot or cold packs are often used in conjunction, to enhance the effect of these modalities. Another available option is therapeutic ultrasound. Ultrasound pushes sound vibrations into tissues. When these vibrations reach your deep tissues, heat develops and unwanted waste products are dispersed.
Myofascial Release
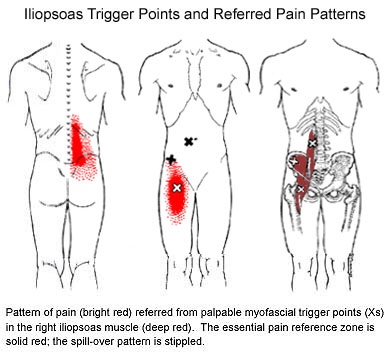
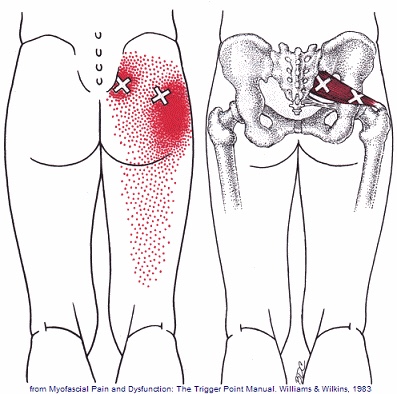
Overworked muscles often become tight and develop knots or “trigger points”. Chronic tightness produces inflammation and swelling that ultimately leads to the formation of “adhesions” between tissues. Your chiropractor will apply pressure with their hands, or with specialized tools, in order to release muscle tightness and soft-tissue adhesions. This will help to improve your circulation, relieve pain and restore flexibility.
Therapeutic Exercise
Muscle tightness or weakness causes discomfort and alters normal joint function, leading to additional problems. Your chiropractor will target tight or weak muscles with specific therapeutic stretching and strengthening to help increase tissue flexibility, build strength, and ease pain. Healthy, strong, and flexible muscles may help prevent re-injury.
Elastic Therapeutic Tape
Your chiropractor may apply a special elastic therapeutic tape in order to support injured areas or encourage better movement. This tape is thought to decrease pain and swelling, improve circulation and limit muscle soreness.
Foot Evaluation
Fallen arches and faulty foot mechanics are common problems that can perpetuate your condition. Our office will carefully evaluate your feet and consider the need for a change in shoe style, arch supports or even custom orthotics.
Ankle Brace
Our office may recommend using a support brace to protect your ankle from further injury. Your doctor will discuss the specific type of brace and provide instructions for use.
|
|
|
After this initial course of treatment we will reassess your progress. We will determine the need for any additional care after your reassessment.
|
 Symptoms include pain on the inner side of your knee, just below the joint. Your pain is probably worse when you stand up or walk stairs. Discomfort increases during activities that require side-to-side movements (i.e. tennis, dancing). Be sure to tell your doctor if you notice clicking, popping, or locking of your knee, excessive thirst, excessive urination, fever, or pain & swelling in your calf.
Symptoms include pain on the inner side of your knee, just below the joint. Your pain is probably worse when you stand up or walk stairs. Discomfort increases during activities that require side-to-side movements (i.e. tennis, dancing). Be sure to tell your doctor if you notice clicking, popping, or locking of your knee, excessive thirst, excessive urination, fever, or pain & swelling in your calf.



 Osgood Schlatter’s disease is more common in athletes, particularly those who participate in soccer, gymnastics, basketball, running or track. It is most common between the ages of 10 and 15 and is relatively equally common between boys and girls. Excessively tight thigh or calf muscles may contribute to this problem.
Osgood Schlatter’s disease is more common in athletes, particularly those who participate in soccer, gymnastics, basketball, running or track. It is most common between the ages of 10 and 15 and is relatively equally common between boys and girls. Excessively tight thigh or calf muscles may contribute to this problem.








