Myofascial pain syndrome (trigger points) and fibromyalgia are often confused to be the same condition and while there is a lot of interrelatedness between the two they are not quite identical. The clinical definition of a trigger point is “a hyper irritable spot associated within a taut band of skeletal muscle that is painful on compression or muscle contraction, and usually responds with a referred pain pattern distant from the spot”. Trigger points form from an overload trauma to the muscle tissue. This is contrasted with fibromyalgia which is defined as “a medical condition characterized by chronic widespread pain and a heightened pain response to pressure. Other symptoms include tiredness to a degree that normal activities are affected, sleep problems and troubles with memory. Some people also report restless leg syndrome, bowel and bladder problems, numbness and tingling and sensitivity to noise, lights and temperature. It is also associated with depression, anxiety, and post traumatic stress disorder”. Fibromyalgia will also present with localized tender points which are often mistaken for trigger points. Where these two conditions become somewhat interrelated is via the nervous system. Fibromyalgia patients suffer from a super-sensitization of the nervous system causing hyperirritability and pain. Myofascial trigger points can be caused by,or be the cause of, super sensitization. An active trigger point will irritate the sensory nerves around it eventually leading to super-sensitization. Trigger points have also been showed to form of become active due to super-sensitization. Both of these conditions can perpetuate the other, leading to layers of pain and symptoms. This being the case, trigger point therapy can have a very positive effect on decreasing the severity of pain and symptoms in patients suffering from fibromyalgia.

Physio
Trigger points in the adductor longus and brevis.
These muscles are located in the groin. The longus originates on the pubic body just below the pubic crest and inserts on the middle third of the linea aspera.The brevis muscle originates on the inferior ramus and body of the pubis and has its attachment to the lesser trochanter and linea aspera of the femur. Trigger points in these muscles are the most common muscular cause of groin pain. Distal trigger points refer pain to the upper medial knee and down the tibia. Proximal trigger points refer into the anterior hip area.
Bryan Cobb RMT.
Since 2005, Bryan has been dedicated to helping all people with chronic and acute pain caused by soft-tissue damage.
His training and experience make him uniquely qualified to treat a wide variety of pain and dysfunction and to give instruction on prevention and self-care.
Bryan is the only Massage Therapist in Manitoba — and one of the few in Canada — to be certified by the Certification Board for Myofascial Trigger Point Therapists (CBMTPT).
Bryan holds a degree as an Advanced Remedial Massage Therapist (ARMT) from the Massage Therapy College of Manitoba. Course work at MTCM includes
• over 2,000 hours of practice, as well as
• intensive course work,
• a supervised clinical practicum, and
• community outreach placements.MTCM has a credit transfer affiliation with the University of Winnipeg, ensuring that its courses are held to the highest level. When Bryan studied at MTCM, the college was the only massage therapy college in western Canada accredited by the Commission on Massage Therapy Accreditation. Today, the college is a member of the Canadian Council of Massage Therapy Schools.
Bryan is a member in good standing of the Natural Health Practitioners of Canada.
Bryan also has a background in Anatomy, Exercise Physiology, and Sport Sciences from the University of Manitoba, and he has worked as a personal trainer and fitness leader.
He is an avid natural bodybuilder and fitness enthusiast, and has a blue belt in Brazilian jiu-jitsu.
Trigger points in the Quadratus Lumborum muscle.
The quadratus lumborum muscle is a commonly overlooked source of low back pain and is often responsible for “pseudo disc syndrome”. This muscle originates on the inferior border of the 12th rib and lumbar transverse processes. It inserts on the iliac crest and iliolumbar ligament. The q.l.’s main actions are extension and lateral flexion of the spine. It also acts as a stabilizer of the lumbar spine. Trigger points in this muscle refer pain into the sacroiliac joint and the lower buttock. Pain can also spread anteriorly along the crest of the ilium into the lower abdomen and groin and to the greater trochanter. 
Want a fancy new hip? Start with this!
A “joint” is an area where two or more bones come together. These bones have a slick rubbery protective covering, called “cartilage,” on the areas where they meet. This cartilage serves as a friction reducer and shock absorber, thereby prolonging the health of our joints.
Osteoarthritis, or simply arthritis, occurs when your joint cartilage degenerates as a result of repetitive stress.

Over time, this cartilage can thin and crack, eventually wearing away, leading to a painful “bone on bone” situation. Thinning of your joint cartilage is often accompanied by the development of “bone spurs” and/or joint deformity further disrupting your joint function.
Hip arthritis is common, affecting up to one-third of the population. The likelihood of you developing osteoarthritis increases as you age, and appears to be at least partially inherited from your parents. It is more common if you have been overweight and if you were subjected to repetitive injury, including occupations & sports requiring prolonged standing or heavy physical exertion.
An early symptom of Hip OA is prolonged stiffness upon arising in the morning and following periods of inactivity. You might complain of the inability to put your socks on, shave your legs or climb stairs. Groin, thigh and buttock pain are common. In some cases the pain can radiate into your lower leg. Cracking and popping of your hip when moving is possible.
It is sometimes difficult for doctors to differentiate between hip osteoarthritis and lower back problems that can also cause hip pain. Your doctor will likely X-ray your hip to determine the extent of your arthritis (graded 1-4 based on severity).
Arthritis cannot be cured, but your symptoms can often be relieved. Treatment of hip arthritis may include exercises, especially water-based programs like “water-aerobics.” Your doctor may use physical therapy modalities and will likely stretch and manipulate your hip, as this has been shown to be effective at relieving symptoms.
Your doctor may recommend that you avoid aggravating activities, especially those requiring you to rotate your hip internally (i.e., pigeon toed” movements), and to maintain a healthy weight. You will be taught home stretching and strengthening exercises to help you recover. Taking 1500 mg of Glucosamine and chondroitin has been shown to help some arthritis sufferers.
In more severe cases, you may need to use a cane (in the opposite hand) to take weight off the arthritic hip. If conservative treatment fails to relieve your pain, your doctor might recommend consultation with an orthopedic hip specialist to consider joint replacement.
Trigger points in the temporalis muscle
The temporalis muscle is located in the temple area of the skull. It originates on the temporal lines on the parietal bone of the skull, and inserts on the coronoid process of the mandible. It’s main action is to close the jaw. The posterior and middle fibres bilaterally retrude the mandible. Acting individually, this muscle will deviate the mandible to the same side. Trigger points in this muscle refer into the teeth causing hypersensitivity, and into and above the eye and temple, causing headaches.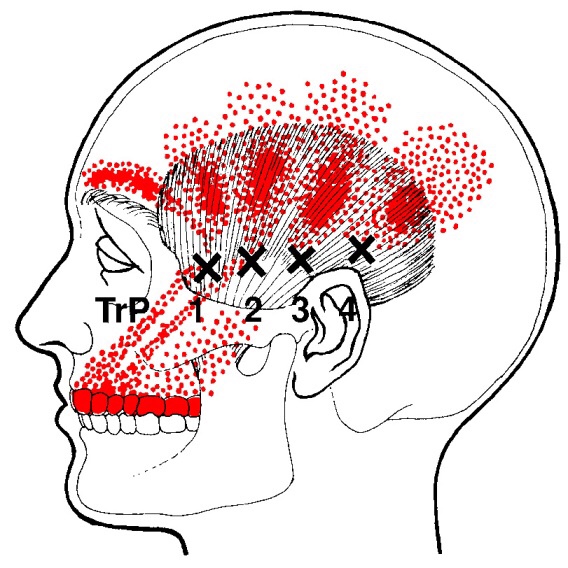
What is Sever’s Disease?
Severs disease, also called calcaneal apophysitis, is a painful swelling near the insertion of the Achilles tendon on your heel.
As our bones develop, we have “growth plates” which are softer areas where the bone is still growing. In children, this growth plate is weaker than in adults. This means that children are more likely to suffer growth plate injuries than adults, especially during periods of rapid growth.

The powerful calf muscles attach onto your heel through the Achilles tendon. When your calf muscle contracts (like during running or jumping), it places a shear force on the growth plate of your heel. Severs disease is an irritation to this sensitive growth plate.
Athletically active children, who run and jump frequently in sports like soccer, basketball, gymnastics and track & field are most likely to suffer from this condition. Severs disease is slightly more common in boys and the condition affects both heels about half of the time.
Symptoms usually start as heel pain that gradually worsens during activity. Sometimes this can cause a “limp”. Rest usually temporarily relieves the pain.
Your doctor will make the diagnosis of Severs disease based on your history and an exam. Your doctor may take an x-ray to rule out other injuries like a stress fracture.
The first goal of treatment is to allow you to return to pain-free activity as soon as possible. This may require avoiding stressful activity like running and jumping for a short period of time. Cross training on a bike is usually acceptable. Ice should be applied for 15 minutes after any activity. You should always wear shoes with good arch supports and avoid walking barefoot. Your doctor may recommend a small heel lift to decrease strain on your achilles tendon.
Trigger points in the lateral pterygoid
The lateral pterygoid muscle plays an important role in prober jaw function. It originates on the greater wing of the sphenoid bone and the lateral pterygoid plate, and inserts on the condyloid process of the mandible. It’s action is to pull the head of the mandibular condyle out of the mandibular fossa while opening the jaw. When trigger points develop they refer pain into the temporal mandibular joint and maxillary sinus. This referral is commonly mistaken for TM arthritis. In addition to the referral pain, trigger points in this muscle can also effect proper movement of the jaw.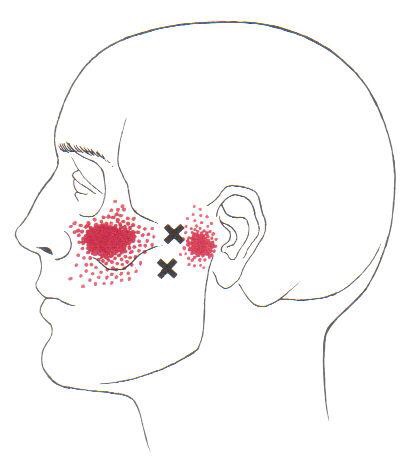

I’ve got Shin Splints; what do I do?
Shin splints, also called “Medial Tibial Stress Syndrome,” (MTSS) is caused when the muscles of your lower leg pull too hard on your bone, causing local pain and inflammation. Over half of all leg pain in athletes is caused from shin splints. Up to 1/3 of runners and soldiers experience shin splints at some point in their lifetime.
MTSS is an overuse injury frequently seen in sports involving running, jumping, or frequent stopping & starting, i.e. field hockey, soccer and cross-country. Shin splints do not occur overnight but over a period of time, often show up during the first two or three weeks of training for a new season. Shin splints can occur when there are changes to your exercise regimen, such as an increase in activity, change in shoes or a change in the surface you play on. Some doctors refer to these training areas as “the terrible toos,” – too much, too hard, too long, too fast.

Symptoms of shin splints include tenderness or pain over the inside lower portion of your shin. The discomfort begins at the start of exercise and eases as you continue. Some patients report “bumps” when touching the inner portion of their leg bone. Be sure to tell your doctor if you experience weakness, numbness or cold feet during exercise or find a very small area of sensitivity.
Unfortunately, MTSS usually develops during a time when you are training heavily for a sport or an upcoming event. Continuing this activity will often lead to ongoing problems and decreased performance. Shin splints are now believed to be a forerunner to stress fracture, so adequate rest is critical. You may need to consider non-weight bearing cross training, such as using a stationary cycle or pool running.
When directed, your return to activity should start slowly, beginning with a 1/4 mile run and progressing by 1/4 mile each time you have no pain for two consecutive workouts. You should initially avoid running on hard or uneven surfaces and begin at a lower intensity and distance, increasing by no more than 10-15% per week- first increase distance, then pace, and avoid hard or unlevel surfaces, including hills.
Sports creams and home ice massage may provide some relief. Use ice after any activity. Patients who have flat feet are predisposed to developing shin splints and may need arch supports or orthotics. Avoid using heel cushions in your shoes, as they may increase the recurrence of this problem.
Trigger points in the serratus anterior
The serratus anterior muscle is located along the sides of the ribs. It originates on the outer surface of the upper 8-9ribs, and inserts on the medial border of the scapula. This muscle acts on the scapula in several different ways. First it rotates the scapula to turn the glenoid fossa upward. It also protracted and elevates the scapula. And lastly it helps to prevent wining. This muscle is often shortened from prolonged sitting and work on a computer. Active trigger points in this muscle refer pain locally around the trigger point with spillover down the inside of the arm. Pain can also radiate into the inferior angle of the scapula. 
