Physio
Chiro & Concussions
Whiplash Associated Disorders (WAD) is the appropriate terminology to use when addressing the myriad of symptoms that can occur as a result of a motor vehicle collision (MVC). In a recent publication in The Physician and Sports Medicine (Volume 43, Issue 3, 2015; 7/3/15 online:1-11), the article “The role of the cervical spine in post-concussive syndrome” takes a look at the neck when it’s injured in a car accident and how this relates to concussion.
It’s estimated about 3.8 million concussion injuries, also referred to as “mild traumatic brain injury” (mTBI), occur each year in the United States. Ironically, it’s one of the least understood injuries in the sports medicine and neuroscience communities. The GOOD NEWS is that concussion symptoms resolve within 7-10 days in the majority of cases; unfortunately, this isn’t the case with 10-15% of patients. Symptoms can last weeks, months, or even years in this group for which the term “post-concussive syndrome” (PCS) is used (defined as three or more symptoms lasting for four weeks as defined by the ICD-10) or three months following a minor head injury (as defined by the Diagnostic and Statistical Manual of Mental Disorders).
There have been significant advances in understanding what takes place in the acute phase of mTBI, but unfortunately, there is no clear physiological explanation for the chronic phase. Studies show the range of force to the head needed to cause concussion is between 60-160g (“g” = gravity) with 96.1g representing the highest predictive value in a football injury, whereas as little as 4.5g of neck acceleration can cause mild strain injury to the neck. In spite of this difference, the signs and symptoms reported by those injured in low-speed MVCs vs. football collisions are strikingly similar!
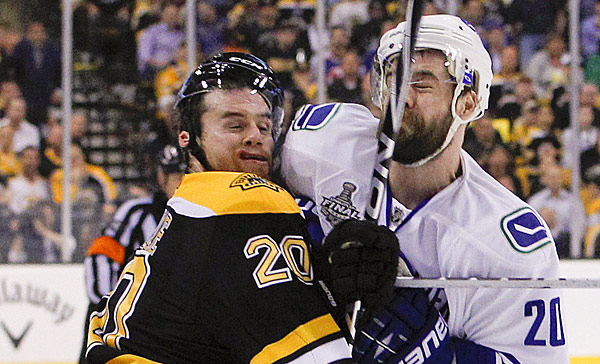
Research shows if an individual sustains an injury where the head is accelerated between 60-160g, it is HIGHLY likely that the tissues of the cervical spine (neck) have also reached their injury threshold of 4.5g. In a study that looked at hockey players, those who sustained a concussion also had WAD / neck injuries indicating that these injuries occur concurrently. Injuries to the neck in WAD include the same symptoms that occur in concussion including headache, dizziness/balance loss, nausea, visual and auditory problems, and cognitive dysfunction, just to name a few.
The paper concludes with five cases of PCS that responded well to a combination of active exercise/rehabilitation AND passive manual therapy (cervical spine manipulation). The favourable outcome supports the concept that the neck injury portion of WAD is a very important aspect to consider when treating patients with PCS!
This “link” between neck injury and concussion explains why chiropractic care is essential in the treatment of the concussion patient! This is especially true when the symptoms of concussion persist longer than one month!
We realize you have a choice in whom you consider for your health care provision and we sincerely appreciate your trust in choosing our service for those needs. If you, a friend, or family member requires care for Whiplash, we would be honoured to render our services.
Exercise Helps LBP!

Moving is good for your back and muscles, especially if you have back pain.
Stiff neck and trigger points.

Myofascial trigger points in the neck muscles are one of the most common causes of neck pain and stiffness. Poor posture and stress can cause muscles in the neck to become overworked and strained. When this happens trigger points will form. These points of contracted muscle will cause pain, referred pain (often into the head), as well as stiffness and weakness. Trigger points won’t resolve on there own, a manual release such as trigger point massage is required to treat the problem.
Brachioradialis trigger points.
The Brachioradialis muscle is a muscle located in your forearm. It helps to flex the elbow during semi pronation, such as when drinking a cup of coffee or holding a phone to your ear. When trigger points form in this muscle pain can be felt in the forearm, back of the elbow, and even into the hand.

Trigger points and myofascial pain.

Sensitive areas of tight muscle fibers can form in your muscles after injuries or overuse. These sensitive areas are called trigger points. A trigger point in a muscle can cause strain and pain throughout the muscle. When this pain persists and worsens, doctors call it myofascial pain syndrome.
What is myofascial pain syndrome?
Myofascial pain syndrome is a chronic pain disorder. In this condition, pressure on sensitive points in your muscles (trigger points) causes pain in the muscle and sometimes in seemingly unrelated parts of your body. This is called referred pain.
This syndrome typically occurs after a muscle has been contracted repetitively. This can be caused by repetitive motions used in jobs or hobbies or by stress-related muscle tension.

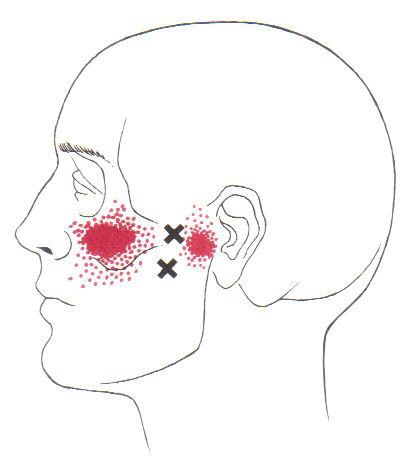
Trigger points in the lateral pterygoid.
The lateral pterygoid muscle is involved in movement of the jaw. It can become become strained from chronic clenching of the jaw and grinding of the teeth. When this happened trigger points can form. This leads not only to pain and refered pain, but also dysfunctional joint mechanics. This muscle is a major player in TMJ dysfunction syndrome.
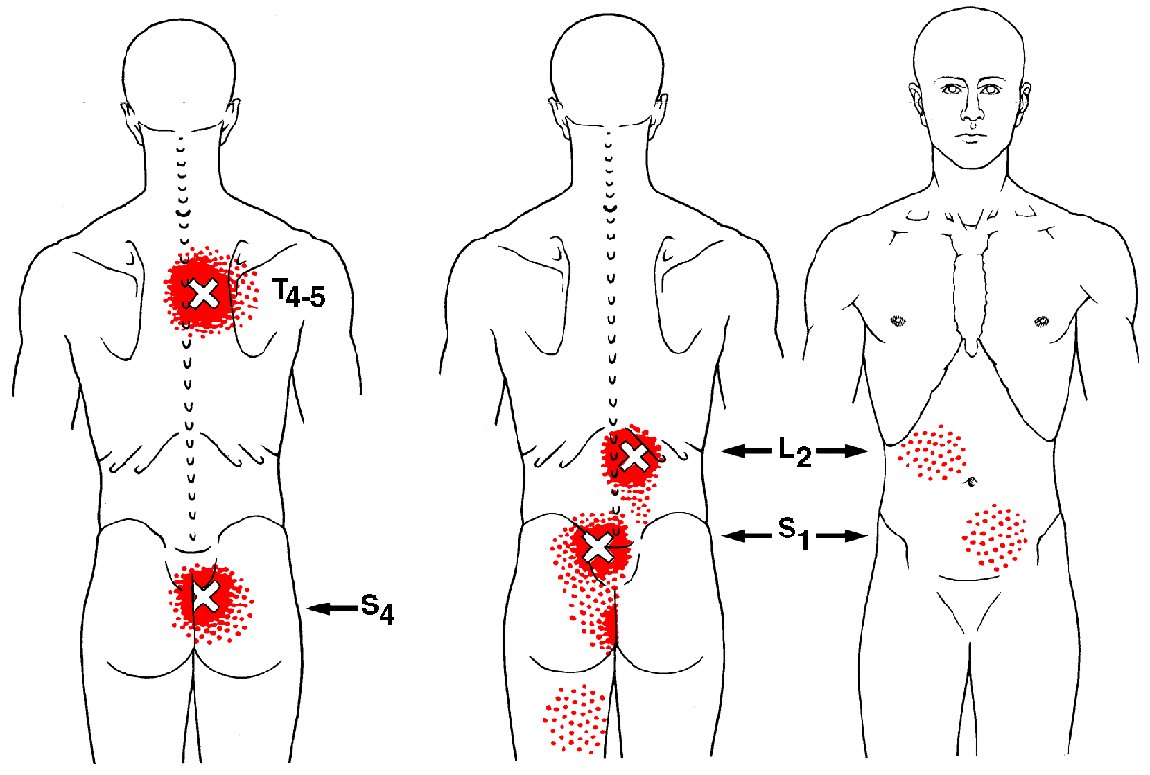
Trigger points in the multifidus muscle.
The multifidus muscle is a long muscle that travels the length of the spine. It has different actions on different parts of the spine. It extends and laterally flexes the cervical and lumbar spine, and rotates the thoracic spine. Trigger points in this muscle are common due to poor posture and bad movement mechanics. Trigger points in the lumbar area area are a common cause of low back pain. These lower points can also refer into the abdomen. Points that form in the cervical region will refer pain down the neck into the shoulder blade area.
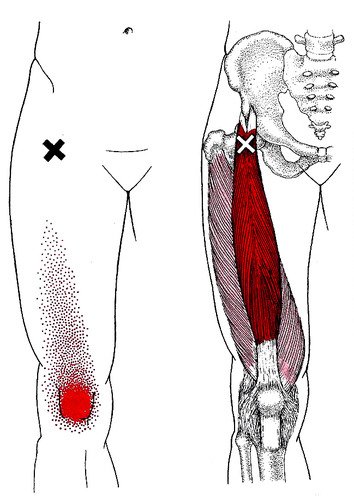
The rectus femoris muscle is one of your quad muscles. It acts primarily to extend the knee but it also helps to flex the hip. This muscle is often overloaded from athletic activity, but it also can become chronically shortened from prolonged sitting. Trigger points will refer pain deep into the knee producing a deep ache felt into the joint.