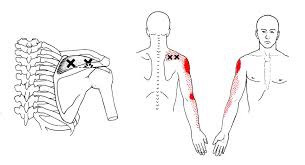
Your shoulder is formed by three bones; the scapula (shoulder blade), the clavicle (collar bone), and the humerus (long arm bone.) These bones come together to form a shallow ball & socket that relies upon the surrounding muscles for support. All of your shoulder muscles must work in a coordinated fashion to have a healthy and stable joint. Disruption of the normal rhythm of your shoulder blade creates abnormal strain on your shoulder and rotator cuff called “Scapular dyskinesis”. This dysfunction crowds the area of your shoulder where your rotator cuff tendons live and may create a painful pinching of your tendons or bursa each time you raise your arm. Many shoulder problems, including sprains/strains, tendinitis, bursitis, or rotator cuff irritation, result from this often overlooked culprit.

Scapular dyskinesis most commonly originates from weakness or imbalance of the muscles that control your shoulder blade. Sometimes the problem is caused by other shoulder conditions like prior fractures, arthritis, or instability. Irritation of the nerves that control the shoulder muscles is the culprit in about 5% of cases.
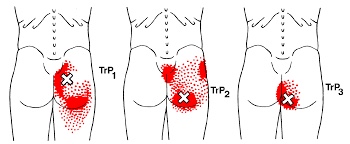
Although scapular dyskinesis can cause a variety of shoulder problems, it may initially go unnoticed. Up to 75% of healthy college athletes show some form of abnormal shoulder blade movement. If the condition is left untreated, you may begin to notice pain near the top of your shoulder. Sometimes the discomfort can radiate toward your neck or into your arm. Patients will often complain of a tender spot on the front of their shoulder. Long-standing altered mechanics can lead to bigger problems, including rotator cuff injury, shoulder instability, and arthritis.
The good news is that we have recognized the underlying cause of your shoulder problems and have treatments to correct it. You will need to perform your exercises consistently. You should also be conscious of your posture and try to avoid sitting or standing in “slouched” positions, as this is known to aggravate your problem.