lifestyle
Carpal Tunnel Syndrome #3

This week, we will conclude our three-part series on important facts regarding carpal tunnel syndrome (CTS).
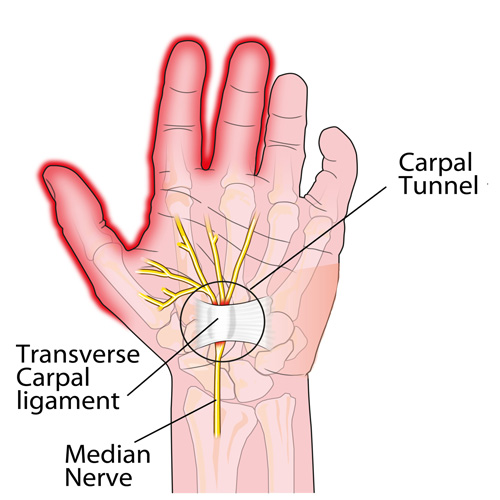
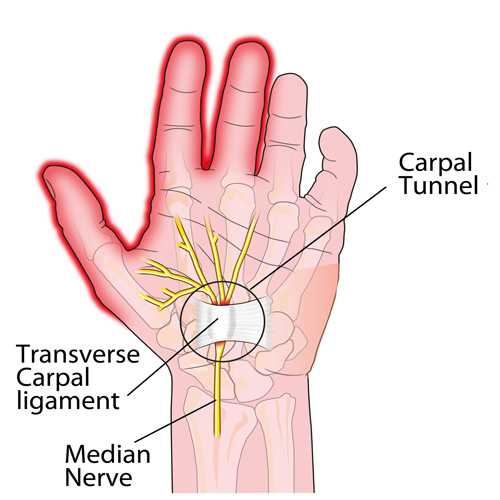
CTS TREATMENT OPTIONS (continued): Aside from the carpal tunnel, there are several places where the median nerve can become compressed as it travels from the neck, down through the shoulder, through tight muscular areas of the upper arm and forearm, and finally through the carpal tunnel at the wrist. In order to achieve good, long-lasting results, treatment must focus on relieving compression at any point along the course of the nerve. This is why chiropractic works SO WELL as it addresses ALL of these areas using manual adjustments, muscle release techniques, and even physical therapy modalities.
CTS PREVENTION: Because there are multiple causes of CTS, prevention must be tailored to each person. For example, if the patient has diabetes mellitus, maintaining a proper blood sugar level is very important because the blood becomes thicker as the sugar levels increase and it simply cannot pass through our small blood vessels (capillaries), especially those located in the feet and hands. This can eventually lead to the need for amputation due to poor circulation and contribute to the numbness associated with diabetic neuropathy.
Similarly, low thyroid function results in a type of swelling called myxedema that can cause or worsen CTS, and keeping the thyroid hormone balanced in the bloodstream is very important. Managing other conditions that create inflammation or swelling, such as rheumatoid and other types of arthritis, will also help prevent CTS from developing or worsening.
Carpal tunnel syndrome can also occur during pregnancy due to the hormonal shifts similar for those taking birth control pills. The PRICE treatment options presented last month can be very helpful for the pregnant mother and represent important non-medication self-care approaches.
Certain occupations that require fast, repetitive work and/or firm gripping can result in carpal tunnel syndrome because of the friction that results in swelling that occurs when the muscle tendons inside the carpal tunnel rub excessively fast together (kind of like starting a fire with two sticks). Modifying the work task until the swelling is controlled is VERY important, as discussed last month.
Other preventative measures include exercises that keep the muscles and tendons in the forearm and inside the carpal tunnel stretched so that the tendons easily slide inside their respective muscle tendon sheaths. This is accomplished by placing the palm side of the hand (elbow straight) on a wall with the fingers pointing downwards while reaching across with the opposite hand and pulling the thumb back until you feel a good firm stretch. Hold this position for 5-10 seconds or until the forearm muscles feel like they are relaxing. Repeat this multiple times a day.
We realize you have a choice in whom you consider for your health care provision and we sincerely appreciate your trust in choosing our service for those needs. If you, a friend, or family member requires care for Carpal Tunnel Syndrome, we would be honored to render our services.
What Exercises Should I Do For Fibro?

Fibromyalgia (FM) is a very common, chronic condition where the patient describes “widespread pain” not limited to one area of the body. Hence, when addressing exercises for FM, one must consider the whole body. Perhaps one of the most important to consider is the squat.
If you think about it, we must squat every time we sit down, stand up, get in/out of our car, and in/out of bed. Even climbing and descending steps results in a squat-lunge type of movement.
The problem with squatting is that we frequently lose (or misuse) the proper way to do this when we’re in pain as the pain forces us to compensate, which can cause us to develop faulty movement patterns that can irritate our ankles, knees, hips, and spine (particularly the low back). In fact, performing a squatting exercise properly will strengthen the hips, which will help protect the spine, and also strengthens the glutel muscles, which can help you perform all the daily activities mentioned above.
The “BEST” type of squat is the free-standing squat. This is done by bending the ankles, knees, and hips while keeping a curve in the low back. The latter is accomplished by “…sticking the butt out” during the squat.
Do NOT allow the knees to drift beyond your toes! If you notice sounds coming from your knees they can be ignored IF they are not accompanied by pain. If you do have pain, try moving the foot of the painful knee about six inches (~15 cm) ahead of the other and don’t squat as far down. Move within “reasonable boundaries of pain” by staying away from positions that reproduce sharp, lancinating pain that lingers upon completion.
Hamstring Problems?

A great injury prevention movement is the glute-ham raise. Done after a warm up and prior to competition it will significantly reduce the odds of hamstring strains in running athletes in sports like Soccer, Football and Sprinting.
To perform the movement:
Begin in a tall kneeling position on a cushion or pillow.
Partner grabs and holds ankles to ground or hook your feet under a stable surface.
Keeping your torso neutral and your thighs in line with your body, bend forward at the knees, using your hamstrings to control the speed of your forward bend.
Go as far as you can without cramping, pain or falling to the ground.
Condition Of The Month: Thoracic Joint Restriction

Your spine is made up of 24 bones stacked on top of each other with a soft “disc” between each segment to allow for flexibility. Normally, each joint in your spine should move freely and independently. When one or more of your spinal vertebra is slightly misaligned and restricted, we call this condition a “spinal segmental joint restriction”. A “thoracic joint restriction” means that this misalignment or restriction is located in your upper or mid-back region.
To help visualize this, imagine a normal spine functioning like a big spring moving freely in every direction. A spine with a joint restriction is like having a section of that spring welded together. The spring may still move as a whole, but a portion of it is no longer functioning.
Joint restrictions can develop in many ways. Sometimes they are brought on by an accident or an injury. Other times, they develop from repetitive strains or poor posture. Being overweight, smoking, strenuous work, and emotional stress can make you more susceptible to problems.
Restricted joints give rise to a self-perpetuating cycle of discomfort. Joint restriction causes swelling and inflammation, which triggers muscular guarding leading to more restriction. Since your spine functions as a unit, rather than as isolated pieces, a joint restriction in one area of your spine often causes “compensatory” problems in another. Think of this as a rowboat with multiple oarsmen on each side. When one rower quits, the others are placed under additional stress and can become overworked.
Joint restrictions most commonly cause local tenderness and discomfort. You may notice that your range of motion is limited. Movement may increase your discomfort. Pain from a restricted joint often trickles around your rib cage or up & down your spine. Be sure to tell your chiropractor if your symptoms include any chest pain, shortness of breath, unusual cough, indigestion or flu- like complaints.
Long-standing restrictions are thought to result in arthritis – much like the way a slightly misaligned wheel on your car causes premature wearing of your tire.
You should recognize that your problem is common and generally treatable. Chiropractic care has been shown to be the safest and most effective treatment for joint restrictions. Our office offers several tools to help ease your pain. To speed your recovery, you should avoid activities that increase your pain. Be sure to take frequent breaks from sedentary activity. Yoga has been shown to help back pain sufferers so consider joining a class or picking up a DVD.
What is CTS?
Why Walk?
What the heck is a trigger point?

What is a Trigger Point?
Trigger Points (TP’s) are defined as a “hyper-irritable spot within a taut band of skeletal muscle. The spot is painful on compression and can evoke characteristic referred pain and autonomic phenomena.”1
Put into plain language, a TP is a painful knot in muscle tissue that can refer pain to other areas of the body. You have probably felt the characteristic achy pain and stiffness that TP’s produce, at some time in your life.
TP’s were first brought to the attention of the medical world by Dr. Janet G. Travell. Dr. Travell, physician to President John F. Kennedy, is the acknowledged Mother of Myofascial Trigger Points. In fact, “Trigger Point massage, the most effective modality used by massage therapists for the relief of pain, is based almost entirely on Dr. Travell’s insights.”2 Dr. Travell’s partner in her research was Dr. David G. Simons, a research scientist and aerospace physician.
Trigger Points are very common. In fact, Travell and Simons state that TP’s are responsible for, or associated with, 75% of pain complaints or conditions.1 With this kind of prevalence, it’s no wonder that TP’s are often referred to as the “scourge of mankind”.
Trigger Points can produce a wide variety of pain complaints. Some of the most common are migraine headaches, back pain, and pain and tingling into the extremities. They are usually responsible for most cases of achy deep pain that is hard to localize.
A TP will refer pain in a predictable pattern, based on its location in a given muscle. Also, since these spots are bundles of contracted muscle fibres, they can cause stiffness and a decreased range of motion. Chronic conditions with many TP’s can also cause general fatigue and malaise, as well as muscle weakness.
Trigger Points are remarkably easy to get, but the most common causes are
TP’s (black X) can refer pain to other areas (red)
Sudden overload of a muscle
- Poor posture
- Chronic frozen posture (e.g., from a desk job), and
- Repetitive strain
Once in place, a TP can remain there for the remainder of your life unless an intervention takes place.
Trigger Points Not Well Known
With thousands of people dealing with chronic pain, and with TP’s being responsible for — or associated with — a high percentage of chronic pain, it is very disappointing to find that a large portion of doctors and other health care practitioners don’t know about TP’s and their symptoms.
Scientific research on TP’s dates back to the 1700’s. There are numerous medical texts and papers written on the subject.
But, it still has been largely overlooked by the health care field. This has led to needless frustration and suffering, as well as thousands of lost work hours and a poorer quality of life.
How Are Trigger Points Treated?
As nasty and troublesome as TP’s are, the treatment for them is surely straight-forward. A skilled practitioner will assess the individual’s pain complaint to determine the most likely location of the TP’s and then apply one of several therapeutic modalities, the most effective of which is a massage technique called “ischemic compression”.
Basically, the therapist will apply a firm, steady pressure to the TP, strong enough to reproduce the symptoms. The pressure will remain until the tissue softens and then the pressure will increase appropriately until the next barrier is felt. This pressure is continued until the referral pain has subsided and the TP is released. (Note: a full release of TP’s could take several sessions.)
Other effective modalities include dry needling (needle placed into the belly of the TP) or wet needling (injection into the TP). The use of moist heat and stretching prove effective, as well. The best practitioners for TP release are Massage Therapists, Physiotherapists, and Athletic Therapists. An educated individual can also apply ischemic compression to themselves, but should start out seeing one of the above therapists to become familiar with the modality and how to apply pressure safely.
1 Simons, D.G., Travell, D.G., & Simons, L.S. Travell and Simons’Myofascial Pain and Dysfunction: the Trigger Point Manual.
Vol. 1. 2nd ed. Lippincott, Williams, and Wilkins, 1999.
Do you have CTS?
Never stop not stopping.

Becoming healthy and staying healthy is hard, challenging work but worth every second of persistence.