The piriformis muscle is a small muscle deep to glute max and lies over top of the sciatic nerve. It originates on the anterior sacrum, and inserts on the greater trochanter of the femur. It’s main action is to laterally rotate the femur. When trigger points developed in this muscle they will refer pain into the sacro-iliac region, across the posterior hip and down the leg. This muscle can also be a cause of sciatic nerve irritation if it gets tight, causing “sciatica” symptoms. 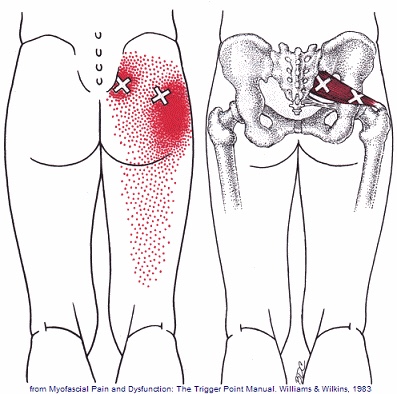
Football
Trigger points in the gluteus minimus
The gluteus minimus is a small but important muscle that lies deep to the gluteus medius. It originates on the gluteal surface of the ilium, and attaches on the greater trochanter of the femur. It’s main actions are to abduct and medically rotate the hip. Trigger points in this muscle refer pain into the buttock and down the lateral and posterior leg, mimicking sciatica. This muscle should be the first to be examined if a straight leg test turns out negative. 
Osgood Schlatter’s Disease
Children and adolescents have soft “growth plates,” which are areas where their bone is still growing. In children, this growth plate is much weaker than in adults. This means that children are more likely to suffer growth plate injuries than adults, especially during periods of rapid growth.
Osgood Schlatter’s disease, also called tibial epiphysitis, is a painful irritation of the growth plate near the insertion of your quadriceps muscle on your knee. The powerful thigh muscles attach onto your knee through the patellar tendon. When your thigh muscle contracts- like during running or jumping, they place a sheer force on the growth plate of your knee.
 Osgood Schlatter’s disease is more common in athletes, particularly those who participate in soccer, gymnastics, basketball, running or track. It is most common between the ages of 10 and 15 and is relatively equally common between boys and girls. Excessively tight thigh or calf muscles may contribute to this problem.
Osgood Schlatter’s disease is more common in athletes, particularly those who participate in soccer, gymnastics, basketball, running or track. It is most common between the ages of 10 and 15 and is relatively equally common between boys and girls. Excessively tight thigh or calf muscles may contribute to this problem.
You may experience pain with activity that requires running or jumping. You will often feel tenderness or even bony enlargement of your “tibial tuberosity”, just below your knee. Kneeling or prolonged squatting may be painful.
Some athletes with mild cases may continue activity as long as it does not increase your symptoms. Most cases may require a period of rest to allow the condition to heal. Depending on the severity of your condition, you may need to limit activities that require running and jumping for a while, usually two to eight weeks. You can often cross train in the pool or on a stationary bike.
You should avoid running with a narrow stride “on a line,” as this may increase your symptoms. Our office may recommend use of a patellar tendon strap to assist with your healing. Osgood Schlatter’s disease can temporarily limit your activity, but most of the time, it can be successfully managed, allowing your return to pain-free activity in a relatively short period of time.
Trigger points in the gluteus medius muscle
The gluteus medius muscle plays an important role in hip and pelvic stability. It originates on the gluteal surface of the ilium, deep to the gluteus Maximus. It inserts on the greater trochanter of the femur. It’s main actions are to abduct the hip and to assist in internal rotation of the hip. It also maintains pelvic stability during walking and running. Trigger points in this muscle will refer pain into the sacrum, the iliac crest, and down the lateral hip and into the thigh. This muscle is often a cause of lower pack pain.
The High Ankle Sprain (Don’t Let This Happen To You. These SUCK.)
Your lower leg bones (tibia and fibula) are held together at the ankle by a group of soft tissues and ligaments called the “syndesmosis”. This connection prevents excessive spreading of these bones during normal activity, but injuries can cause these ligaments to be stretched or torn. This problem is called a “syndesmotic ankle sprain” or “high ankle sprain”. High ankle sprains often occur during contact sports (like football, hockey, and soccer) when your foot is planted while the rest of your body shifts forward and turns inward. High ankle sprains are much less common than other types of ankle sprains.

The pain of a high ankle sprain starts just above your ankle and runs up your shin. Interestingly, the “length” of pain correlates very closely to your severity of injury. Standing and walking is usually uncomfortable and sometimes unbearable. Bringing your toes toward your shin or rotating your foot outward will likely increase your pain. Significant bruising or swelling is possible. Be sure to tell your doctor if you notice numbness, tingling, or coldness in your foot.
Ankles that have suffered a complete separation usually require surgery, since they will have lost the ability to push off, propel, and cut. Most other stable sprains will respond to conservative care, like the type provided in this office. It is important to recognize that high ankle sprains heal more slowly than other types of ankle sprains. The average recovery time for a syndesmotic sprain is between two and seven weeks but some injuries may require up to four months away from your sport. You may need to wear a boot or avoid weight bearing for a period of time. Ice may help to limit swelling initially, and the home exercises described below are an important part of your recovery.
Achilles Tendonitis: The Details
Your Achilles tendon is the strong fibrous band of tissue that connects your calf muscles to your heel. The tendon is named after “Achilles” who was a powerful, yet vulnerable warrior in Greek mythology. Likewise, our Achilles tendon, being the largest and strongest tendon in the body, is susceptible to injury from the high demands placed on it. (Running can generate forces over 12 times your bo

dy weight on the Achilles tendon.)
The tendon may be strained or even ruptured from excessive stretch or forceful contraction of the calf muscles. More commonly, the tendon is repeatedly overloaded and suffers tiny “micro tears.” Damage usually occurs either directly behind the heel, or near the weakest area of the tendon- one to two inches above the heel.
Achilles tendon injuries affect between 250,000 and 1 million people per year. Most are middle-aged males, between the age of 30 and 50. Interestingly, Achilles tendon injuries occur more frequently on the left side. If you have suffered a prior Achilles tendon injury, you are at greater risk of injuring the opposite side. Two-thirds of all Achilles tendon injuries involve athletes. Runners are up to 10 times more likely to suffer Achilles tendon problems. You may at increased risk if the arch of your foot is too high or too flat.
Symptoms may begin abruptly following a strain but more commonly develop slowly from repeated irritation. Morning pain and stiffness are common. Your symptoms will likely increase with activity, especially walking or running. You may notice pain when you rise up on your toes. Walking down stairs stretches the tendon and usually increases symptoms. Some patients notice that the irritated area becomes firmly swollen. Ongoing irritation to the spot on your heel where the tendon inserts can cause a painfully elevated “pump bump.”
Research has shown that conservative care, like the type provided in this office, can produce “excellent results” in over 85% of patients. Initially, you may need to limit or stop activities that cause pain. Runners may need to switch to swimming or cycling for a short period of time. Be sure to introduce new activities slowly and avoid increasing your activity by more than 10% per week. Runners should begin on a smooth, shock-absorbent surface and start at a low intensity – first increasing distance, then pace. Avoid training on hard or unlevel surfaces like hills. Make sure you warm up properly and avoid over training. Avoid wearing high heels or shoes with an excessively rigid heel tab. One of the most important and effective treatments for Achilles tendinopathy is performing “heel drop exercises” as outlined below.
Here is a brief description of the treatments we may use to help manage your problem.
 Joint Manipulation
Your chiropractor has found joints in your body that are not moving freely. This can cause tightness and discomfort and can accelerate unwanted degeneration i.e. arthritis. Your chiropractor will apply a gentle force with their hands, or with hand held instruments, in order to restore motion to any “restricted” joints. Sometimes a specialized table will be used to assist with these safe and effective “adjustments”. Joint manipulation improves flexibility, relieves pain and helps maintain healthy joints.
 Therapy Modalities
We may apply electrotherapy modalities that produce light electrical pulses transmitted through electrodes placed over your specific sites of concern. These comfortable modalities work to decrease your pain, limit inflammation and ease muscle spasm. Hot or cold packs are often used in conjunction, to enhance the effect of these modalities. Another available option is therapeutic ultrasound. Ultrasound pushes sound vibrations into tissues. When these vibrations reach your deep tissues, heat develops and unwanted waste products are dispersed.
 Myofascial Release
Overworked muscles often become tight and develop knots or “trigger points”. Chronic tightness produces inflammation and swelling that ultimately leads to the formation of “adhesions” between tissues. Your chiropractor will apply pressure with their hands, or with specialized tools, in order to release muscle tightness and soft-tissue adhesions. This will help to improve your circulation, relieve pain and restore flexibility.
 Therapeutic Exercise
Muscle tightness or weakness causes discomfort and alters normal joint function, leading to additional problems. Your chiropractor will target tight or weak muscles with specific therapeutic stretching and strengthening to help increase tissue flexibility, build strength, and ease pain. Healthy, strong, and flexible muscles may help prevent re-injury.
 Elastic Therapeutic Tape
Your chiropractor may apply a special elastic therapeutic tape in order to support injured areas or encourage better movement. This tape is thought to decrease pain and swelling, improve circulation and limit muscle soreness.
 Foot Evaluation
Fallen arches and faulty foot mechanics are common problems that can perpetuate your condition. Our office will carefully evaluate your feet and consider the need for a change in shoe style, arch supports or even custom orthotics.
 Ankle Brace
Our office may recommend using a support brace to protect your ankle from further injury. Your doctor will discuss the specific type of brace and provide instructions for use.
|
||
|
After this initial course of treatment we will reassess your progress. We will determine the need for any additional care after your reassessment.
|
||
Trigger points in the gluteus Maximus
The gluteus Maximus is the buttock muscle. It originates on the gluteal surface of the ilium, lumbar fascia, sacrum and sacrotuberous ligament. It inserts on the gluteal tuberosity of the femur and the iliotibial tract. Extension and lateral rotation of the hip are it’s main actions. This muscle is heavily involved in activities like ice skating and is a common area to develops trigger points. When trigger points do develop they can refer pain in a crescent pattern from the gluteal fold to the sacrum. Trigger points can also refer pain deep into the buttock itself making it feel like other deeper muscles are involved. These symptoms can sometimes be mistaken for s.i. Joint problems. 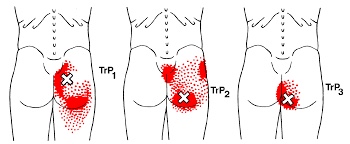
SI Joint Dysfunction. Nothing FUN about it.
Your sacroiliac joint is the mechanical link on each side of your hip that connects your legs to the rest of your body. The joint has a limited but very important degree of mobility. Symptoms develop when one or both of the joints loses normal motion. When a joint becomes “restricted”, a self-perpetuating cycle of discomfort follows. Restriction causes the muscles to become overworked, leading to tightness, compression, inflammation, pain and more restriction.
 Sacroiliac problems can happen as a result of repetitive strenuous activity or trauma- like a fall onto the buttocks. Other causes of sacroiliac joint problems include, poor posture, having one leg slightly longer than another, having an altered gait, having flat feet or scoliosis, or having pain somewhere else in your legs. Pregnancy is a common trigger for sacroiliac joint problems due to weight gain, gait changes and postural stress.
Sacroiliac problems can happen as a result of repetitive strenuous activity or trauma- like a fall onto the buttocks. Other causes of sacroiliac joint problems include, poor posture, having one leg slightly longer than another, having an altered gait, having flat feet or scoliosis, or having pain somewhere else in your legs. Pregnancy is a common trigger for sacroiliac joint problems due to weight gain, gait changes and postural stress.
Sacroiliac joint problems often begin as a focal discomfort in your back just below the belt line, slightly to one side of center. Your pain can travel into your buttock or thigh. Symptoms are often worse by standing on the affected side. The pain may become more apparent when you change positions- like exiting a chair, car or bed, or during long car rides. The pain is often relieved by lying down.
To assist with your recovery, you should avoid any activity that provokes pain, like standing on the affected leg or prolonged sitting.
Turf Toe? What Is That?
“Turf toe” means that the strong fibrous ligaments connecting your big toe to your foot have been stretched too far and have been “sprained.” This most commonly happens when your big toe is extended forcibly toward the top of your foot. This may happen abruptly from a fall or when something lands on the back of your calf while your toes are touching the ground. Turf toe commonly occurs from jamming your big toe into a hard surface. Occasionally, the injury happens over a long period of time from repetitive stress- like pushing off of the big toe each time you run or jump.

The term “turf toe” was coined because this injury became more common in athletes with the implementation of artificial turf fields. Turf toe injuries rank third after knee and ankle injuries among the most common cause for lost playing time in athletes.
A turf toe injury causes pain and swelling at the base of your big toe. You will notice your pain probably increases when your toe is straightened or bent backward toward the top of your foot. Sometimes you may notice bruising shortly after the injury. Gout, a type of arthritis that is more common in men, can sometimes act like turf toe. Be sure to tell your doctor if you or someone in your family has a history of gout.
Early treatment is focused on keeping your toe from moving too much. Depending upon the severity of the injury, turf toe usually requires a period of rest for proper healing. When directed, you may begin non-weight bearing activities, such as stationary cycling or swimming. You should take a close look at your shoes before returning to play. Wearing excessively flexible shoes on a turf field increases your chance of injury. Consider a stiff-soled shoe or hard carbon fiber insert during initial healing. When you are able to run and change directions without pain or loss of mobility, you will likely be allowed to return to play. Be sure to ice your toe for 10-15 minutes following any activity while your injury is healing.
The Dreaded Lateral Ankle Sprain
“Ligaments” are made up of many individual fibers running parallel to each other and bundled to form a strong fibrous band. These fibrous bands hold your bones together. Just like a rope, when a ligament is stretched too far, it begins to fray or tear. “Sprain” is the term used to describe this tearing of ligament fibers.
Sprains are graded by the severity of damage to the ligament fibers. A Grade 1 sprain means the ligament has been painfully stretched, but no fibers have been torn. A Grade 2 sprain means some, but not all, of the ligaments’ fibers have been torn. A Grade 3 sprain means all of the ligaments’ fibers have been torn, and the ligament no longer has the ability to protect the joint.


Ankle sprains are the most common soft-tissue injury and will affect up to 20% of active people at some point in their life. Most ankle sprains occur because you have “rolled your ankle” inward. Sprains on the outer side of your ankle are much more common than sprains on the inner side. People who have suffered a prior ankle injury are more likely to suffer subsequent ankle injuries.
Ankle sprains cause pain and swelling over the outside of your ankle. Walking may be difficult, and bruising is common. Be sure to tell your doctor if you experience numbness, tingling, or a dramatic cold sensation in your foot, as this may indicate more significant injury.
Ankle sprains can be successfully managed but will require some work on your part. You can help reduce swelling by elevating your ankle by lying or sitting with your foot elevated or by using an ACE wrap for compression. Applying ice or ice massage for 10 minutes each hour may help relieve swelling. Depending upon the severity of your sprain, you may need to wear an ankle brace to help protect you from further injury. If walking is painful, crutches may be necessary.
Initially, a period of rest may be necessary in order to help you heal. Mild Grade 1 sprains may allow return to sport in a couple of days, while more severe injuries may take six weeks or longer to recover. Surgery is rarely necessary.
