The muscles of the hip provide not only local stability, but also play an important role in spinal and lower extremity functional alignment. (1-4) While weakness in some hip muscles (hip extensors and knee extensors) is well tolerated, weakness or imbalance in others can have a profound effect on gait and biomechanical function throughout the lower half of the body. (5) Weakness of the hip abductors, particularly those that assist with external rotation, has the most significant impact on hip and lower extremity stability. (5,6)
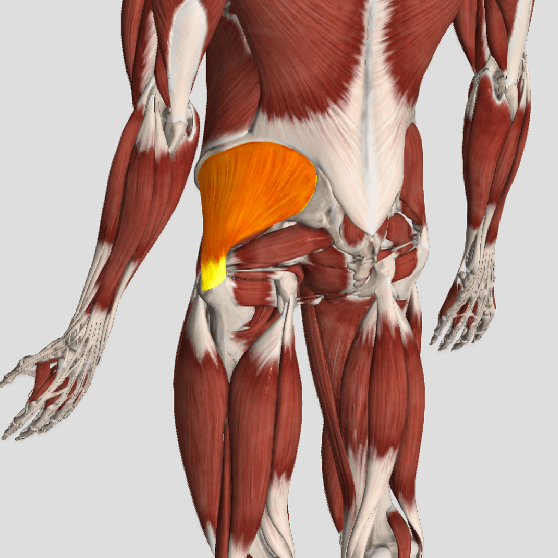
The gluteus medius is the principal hip abductor. When the hip is flexed, the muscle also assists the six deep hip external rotators (piriformis, gemelli, obturators, and quadratus femoris). The gluteus medius originates on the ilium just inferior to the iliac crest and inserts on the lateral and superior aspects of the greater trochanter. While the principal declared action of the gluteus medius is hip abduction, clinicians will appreciate its more valuable contribution as a dynamic stabilizer of the hip and pelvis- particularly during single leg stance activities like walking, running, and squatting. The gluteus medius contributes approximately 70% of the abduction force required to maintain pelvic leveling during single leg stance. The remainder comes predominantly from 2 muscles that insert onto the iliotibial band: the tensor fascia lata and upper gluteus maximus. Hip abductor strength is the single greatest contributor to lower extremity frontal plain alignment during activity. (6)
Incompetent hip abductors and/or external rotators allows for excessive adduction and internal rotation of the thigh during single leg stance activities. This leads to a cascade of biomechanical problems, including pelvic drop, excessive hip adduction, excessive femoral internal rotation, valgus knee stress, and internal tibial rotation. (1,7-12)