This muscle originates on the bodies and disks of T12-L5 and the inner ilium. It inserts on the lesser trochanter of the femur. The psoas flexes the hip when the spine is fixed. When the leg is fixed it extends the lumbar spine increasing lumbar lordosis. This Muscle is often chronically shortened due to inactivity and sitting posture. When trigger points are present they will refer pain primarily to the lower lumbar area and the sacrum as well as into the anterior thigh. Trigger points in the iliopsoas muscle can mimic appendicitis.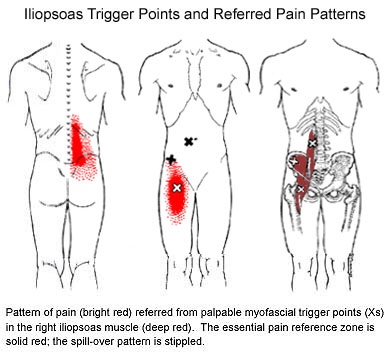
Fibromyalgia
Trigger points in the piriformis muscle
The piriformis muscle is a small muscle deep to glute max and lies over top of the sciatic nerve. It originates on the anterior sacrum, and inserts on the greater trochanter of the femur. It’s main action is to laterally rotate the femur. When trigger points developed in this muscle they will refer pain into the sacro-iliac region, across the posterior hip and down the leg. This muscle can also be a cause of sciatic nerve irritation if it gets tight, causing “sciatica” symptoms. 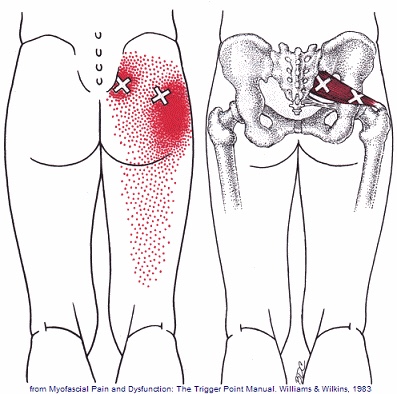
Trigger points in the gluteus minimus
The gluteus minimus is a small but important muscle that lies deep to the gluteus medius. It originates on the gluteal surface of the ilium, and attaches on the greater trochanter of the femur. It’s main actions are to abduct and medically rotate the hip. Trigger points in this muscle refer pain into the buttock and down the lateral and posterior leg, mimicking sciatica. This muscle should be the first to be examined if a straight leg test turns out negative. 
Trigger points in the gluteus medius muscle
The gluteus medius muscle plays an important role in hip and pelvic stability. It originates on the gluteal surface of the ilium, deep to the gluteus Maximus. It inserts on the greater trochanter of the femur. It’s main actions are to abduct the hip and to assist in internal rotation of the hip. It also maintains pelvic stability during walking and running. Trigger points in this muscle will refer pain into the sacrum, the iliac crest, and down the lateral hip and into the thigh. This muscle is often a cause of lower pack pain.
Trigger points in the gluteus Maximus
The gluteus Maximus is the buttock muscle. It originates on the gluteal surface of the ilium, lumbar fascia, sacrum and sacrotuberous ligament. It inserts on the gluteal tuberosity of the femur and the iliotibial tract. Extension and lateral rotation of the hip are it’s main actions. This muscle is heavily involved in activities like ice skating and is a common area to develops trigger points. When trigger points do develop they can refer pain in a crescent pattern from the gluteal fold to the sacrum. Trigger points can also refer pain deep into the buttock itself making it feel like other deeper muscles are involved. These symptoms can sometimes be mistaken for s.i. Joint problems. 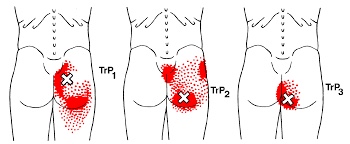
Trigger points in the supraspinatus
The supraspinatus is a muscle of the rotator cuff. Is sits above the infraspinatus and originates on the supraspinous fossa of the scapula. It’s insertion point is the superior facet of the greater tubercle of the humerus. It’s main function is to abduct the arm at the glenohumeral joint working with the deltoid. All rotator cuff muscles act to secure and support the head of the humerus in the glenoid fossa during arm movements acting as a sling. This muscle often gets impinged during overhead movements such as painting a ceiling. When trigger points form in this muscle they primarily refer a deep achy pain into the mid deltoid area with spillover pain radiating down the arm into the elbow.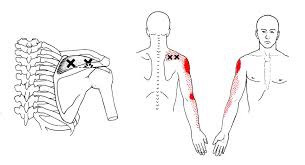
Can Chiro help me?

Chiropractic is the most widely accepted and most frequently used type of “alternative” healthcare in the United States. This is largely due to the fact that it works, and because of that, there has been a steady increase in acceptance by the public, third-party payers, and the Federal government. Since the mid-1990s, a number of outside (non-chiropractic) observers have suggested that chiropractic has now entered mainstream healthcare.
One can position chiropractic as being BOTH alternative and mainstream. It is “alternative” since it approaches healthcare from an entirely different direction compared to the primary care medical profession. Chiropractic is non-surgical and promotes diet and nutritional approaches vs. drugs and surgery. Chiropractic is also arguably “mainstream” as it has evolved into a strongly utilized form of primary care through popular acceptance and utilization by the public.
So, what role does chiropractic play in today’s health delivery system? This question is still being debated, but there appears to be three camps: 1) Specialist—limited to musculoskeletal (MSK) complaints on an interdisciplinary primary healthcare team; 2) Primary healthcare “gatekeepers” that focus on ambulatory MSK complaints; 3) Generalist primary healthcare provider of “alternative or complementary” medicine that manage and/or co-manage both MSK AND non-MSK conditions.
Looking at this from the patient or “consumer” perspective, chiropractic already plays an important role in the healthcare delivery for many patients. In 1993, a report claimed 7% of American adults had received chiropractic care during the prior year. According to a 2015 Gallup poll (that included 5,442 adults, aged 18+, surveyed between 2/16/15 and 5/6/15) entitled, Majority in U.S. Say Chiropractic Works for Neck, Back Pain, “Chiropractic care has a positive reputation among many US adults for effective treatment of neck and back pain, with about six in 10 adults either strongly agreeing (23%) or agreeing somewhat (38%) that chiropractors are effective at treating these types of pain.”
The “highlights” from this Gallup poll include: 1) Two-thirds say chiropractic is effective for neck and back pain. 2) Many adults say chiropractors think of the patient’s best interest. 3) More than 33 million adults in the United States (US) saw a chiropractor in the twelve months before the survey was conducted. That means roughly 14% of U.S. adults saw a chiropractor in the 12 months prior to the survey (vs. 7% in 1993). An additional 12% who responded to the Gallup pollsters saw a chiropractor in the last five years but not in the last 12 months. Overall, 51% of those polled had previously seen a chiropractor.
Whether or not you have personally utilized chiropractic, the educational process, licensing requirements, public interest, third-party payer systems, and interprofessional cooperation ALL support firm ground for which you can comfortably and confidently seek chiropractic care for your complaints.
We realize you have a choice in whom you consider for your health care provision and we sincerely appreciate your trust in choosing our service for those needs. If you, a friend, or family member requires care, we would be honored to render our services.
Trigger points in the infraspinatus
The infraspinatus muscle is one of the muscles that makes up the rotator cuff. It originates on the infraspinous fossa of the scapula, and inserts on the middle facet of the greater tubercle of the humerus. It functions to externally rotate the humerus and to stabilize the head of the humerus in the glenoid cavity during upward movement of the arm. Trigger points in this muscle refer pain deep into the anterior shoulder joint and down the anterior arm. Trigger points near the lower medial border refer pain into the rhomboids. This muscle is often injured during throwing motions.
Is there an actual cure all?
No; but exercise seems to be as close as we will ever get!
Some of you may have heard about how a modified form of boxing is helping patients with Parkinson’s disease (PD). If you haven’t, it’s been observed that people with Parkinson’s disease (PD) who engage in this boxing-like exercise routine can enhance their quality of life and even build impressive gains in posture, strength, flexibility, and speed. Proponents of the program report that regardless the degree of severity of PD, participants have a happier, healthier, and higher quality of life.
But must it be boxing? Maybe not. A report presented at the International Congress of Parkinson’s Disease and Movement Disorders in San Diego in June 2015 found that patients with Parkinson’s disease who began regular exercise early into the PD process had a much slower decline in their quality of life when compared with those who started exercising later. The researchers found just 2.5 hours per week of exercise is needed to improve quality of life scores. According to the report, it didn’t matter what exercise the participants did — simply getting up and moving for a total of 2.5 hours/week was reportedly enough (that’s only 20-25 minutes / day)!
Looking beyond Parkinson’s, other chronic conditions also benefit from adding exercise into a person’s lifestyle. Studies show that regular exercise as simple as walking helps reduce one’s risk for memory loss, and it slows down functional decline in the elderly. Incorporating aerobic exercise into one’s lifestyle can also improve reaction time in people at ALL AGES. Exercise has also been shown to improve both physical and emotional well-being in those afflicted with Alzheimer’s disease with as little as 60 minutes/week of moderate exercise! Patients with multiple sclerosis (MS) have also reported less stiffness and less muscle wasting when using exercise machines, aquatic exercise, and/or walking.
Research has shown just 30 minutes of brisk exercise three times a week can help reduce depressive symptoms in patients with mild-to-moderate depression. In a study involving teenagers, those who engaged in sports reported a greater level of well-being than their sedentary peers, and the more vigorous the exercise, the better their emotion health! In kids 8-12 years old, physical inactivity is strongly linked to depression.
Even anxiety, stress, and depression associated with menopause are less severe in those who exercise! So LET’S ALL GET OUT THERE AND EXERCISE!!!
Trigger points in the triceps muscle.
The tricep muscle is named for its three heads long, medial, and lateral. The long head originates on the infraglenoid tubercle, the medial head on the posterior humerus, and the lateral head on the posterior humerus as well. They join together to insert on the Olecranon process of the ulna. The triceps function to extend the elbow. Strong extension under resistance can cause trigger points to form. Pain referred from triceps trigger points can be felt in the posterior shoulder and down the posterior forearm, as well as in in the olecranon process and the lateral epicondyle which can cause “tennis elbow” pain.

