CTS
Carpal Tunnel Syndrome #3

This week, we will conclude our three-part series on important facts regarding carpal tunnel syndrome (CTS).
CTS TREATMENT OPTIONS (continued): Aside from the carpal tunnel, there are several places where the median nerve can become compressed as it travels from the neck, down through the shoulder, through tight muscular areas of the upper arm and forearm, and finally through the carpal tunnel at the wrist. In order to achieve good, long-lasting results, treatment must focus on relieving compression at any point along the course of the nerve. This is why chiropractic works SO WELL as it addresses ALL of these areas using manual adjustments, muscle release techniques, and even physical therapy modalities.
CTS PREVENTION: Because there are multiple causes of CTS, prevention must be tailored to each person. For example, if the patient has diabetes mellitus, maintaining a proper blood sugar level is very important because the blood becomes thicker as the sugar levels increase and it simply cannot pass through our small blood vessels (capillaries), especially those located in the feet and hands. This can eventually lead to the need for amputation due to poor circulation and contribute to the numbness associated with diabetic neuropathy.
Similarly, low thyroid function results in a type of swelling called myxedema that can cause or worsen CTS, and keeping the thyroid hormone balanced in the bloodstream is very important. Managing other conditions that create inflammation or swelling, such as rheumatoid and other types of arthritis, will also help prevent CTS from developing or worsening.
Carpal tunnel syndrome can also occur during pregnancy due to the hormonal shifts similar for those taking birth control pills. The PRICE treatment options presented last month can be very helpful for the pregnant mother and represent important non-medication self-care approaches.
Certain occupations that require fast, repetitive work and/or firm gripping can result in carpal tunnel syndrome because of the friction that results in swelling that occurs when the muscle tendons inside the carpal tunnel rub excessively fast together (kind of like starting a fire with two sticks). Modifying the work task until the swelling is controlled is VERY important, as discussed last month.
Other preventative measures include exercises that keep the muscles and tendons in the forearm and inside the carpal tunnel stretched so that the tendons easily slide inside their respective muscle tendon sheaths. This is accomplished by placing the palm side of the hand (elbow straight) on a wall with the fingers pointing downwards while reaching across with the opposite hand and pulling the thumb back until you feel a good firm stretch. Hold this position for 5-10 seconds or until the forearm muscles feel like they are relaxing. Repeat this multiple times a day.
We realize you have a choice in whom you consider for your health care provision and we sincerely appreciate your trust in choosing our service for those needs. If you, a friend, or family member requires care for Carpal Tunnel Syndrome, we would be honored to render our services.
Carpel Tunnel in a nutshell
Here it is: carpal tunnel syndrome (CTS) in a nutshell!
What is CTS?
Do you have CTS?
Carpal Tunnel Syndrome
| Carpal Tunnel Syndrome |
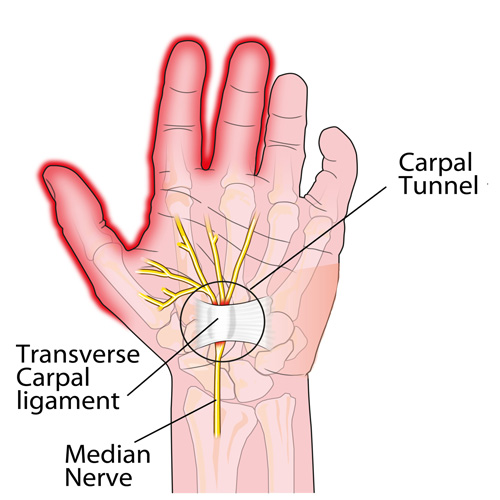
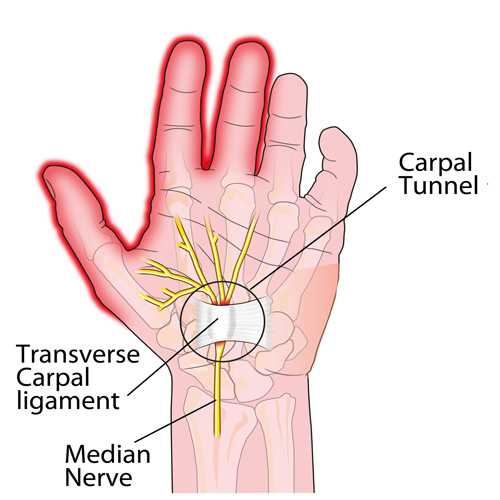
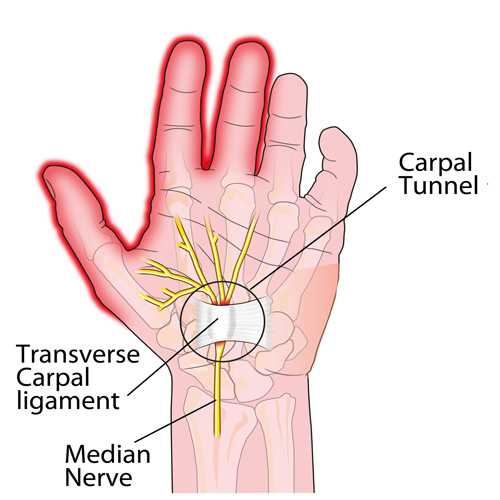
| Carpal tunnel syndrome is a compression or irritation of the median nerve at the carpal tunnel on the anterior side of the wrist.This condition is usually the result of repetitive wrist movement, such as regular and prolonged use of a computer mouse or repetitive movements at work. Carpal tunnel syndrome can also occur as a result of trauma or tendinitis of the flexor muscles of the wrist, or during pregnancy due to nerve compression as a result of swelling in the hands.It is estimated that about 8% of the adult population is affected, making it a relatively common condition. It is the most common compression neuropathy of the upper limb. Women are twice as affected as men. Structures involvedThe nerves of the hand as well as the tendons of the flexor muscles pass to the anterior aspect of the wrist under the transverse carpal ligament that holds them in place. It is the passage formed by the transverse ligament and the bones of the wrist, called carpal bones, that forms the carpal tunnel. The syndrome usually occurs when, for some reason, the space in the carpal tunnel is reduced and the median nerve is compressed.In some cases, a dysfunction of the cervical spine can cause symptoms of carpal tunnel syndrome without repetitive wrist extension motion. |
▬▬▬▬▬
Signs & Symptoms that you may experience
Carpal tunnel syndrome can cause, but is not limited to, numbness and tingling in the first three fingers and half of the fourth, as well as atrophy of the hand muscles. During the night, you may experience pain and numbness from prolonged bending of the wrist. Symptoms are also exacerbated during repetitive activities involving wrist movements.
▬▬▬▬▬
Recovery
Your rehabilitation plan, health profile, fitness level and nutritional status affect the recovery time. Most of the time, you should recover completely from carpal tunnel syndrome. This condition may take a few months to fully recover.
▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬▬
▶ WHAT TO DO
Early Stage
Relative rest is a good way to protect your carpal tunnel syndrome and prevent your injury from getting worse, but it is important to avoid over-protecting it. A few days of rest by reducing activities that cause pain may be necessary. A quick return to your daily activities, light cardiovascular exercise and specific mobility and strengthening exercises will allow for better recovery.
Follow your therapist’s advice. This will help you manage the various stages of the healing process and increase the odds of successful rehabilitation. Your therapist will accompany you during your rehabilitation program to restore your joint range of motion, muscle strength and endurance, flexibility and functional status.
According to the principles of carpal tunnel rehabilitation, reducing aggravating factors and recovering neural mobility, through neurodynamic exercises, would be an important part of functional recovery.
▶ WHAT TO AVOID
Do not rely solely on a passive treatment approach. Each phase of the rehabilitation process is important. Patients who actively participate in their treatment plan tend to recover more quickly. As soon as you feel better and the pain is well under control, introduce, in collaboration with your therapist, mild strengthening exercises based on your tolerance.
CTS Warning Signs
Headaches are REALLY common! In fact, two out of three children will have a headache by the time they are fifteen years old, and more than 90% of adults will experience a headache at some point in their life. It appears safe to say that almost ALL of us will have firsthand knowledge of what a headache is like sooner or later!
Certain types of headaches run in families (due to genetics), and headaches can occur during different stages of life. Some have a consistent pattern, while others do not. To make this even more complicated, it’s not uncommon to have more than one type of headache at the same time!
Headaches can vary in frequency and intensity, as some people can have several headaches in one day that come and go, while others have multiple headaches per month or maybe only one or two a year. Headaches may be continuous and last for days or weeks and may or may not fluctuate in intensity.
For some, lying down in a dark, quiet room is a must. For others, life can continue on like normal. Headaches are a major reason for missed work or school days as well as for doctor visits. The “cost” of headaches is enormous—running into the billions of dollars per year in the United States (US) in both direct costs and productivity losses. Indirect costs such as the potential future costs in children with headaches who miss school and the associated interference with their academic progress are much more difficult to calculate.
There are MANY types of headaches, which are classified into types. With each type, there is a different cause or group of causes. For example, migraine headaches, which affect about 12% of the US population (both children and adults), are vascular in nature—where the blood vessels dilate or enlarge and irritate nerve-sensitive tissues inside the head. This usually results in throbbing, pulsating pain often on one side of the head and can include nausea and/or vomiting. Some migraine sufferers have an “aura” such as a flashing or bright light that occurs within 10-15 minutes prior to the onset while other migraine sufferers do not have an aura.
The tension-type headache is the most common type and as the name implies, is triggered by stress or some type of tension. The intensity ranges between mild and severe, usually on both sides of the head and often begin during adolescence and peak around age 30, affecting women slightly more than men. These can be episodic (come and go, ten to fifteen times a month, lasting 30 min. to several days) or chronic (more than fifteen times a month over a three-month period).
There are many other types of headaches that may be primary or secondary—when caused by an underlying illness or condition. The GOOD news is chiropractic care is often extremely helpful in managing headaches of all varieties and should be included in the healthcare team when management requires a multidisciplinary treatment approach.
Can Carpal Tunnel Be Prevented?
Carpal Tunnel Syndrome (CTS) is a VERY common condition where the median nerve is compressed or squeezed as it passes through the wrist. One reason that it’s so common is because MANY daily activities require fast, repetitive use of the fingers, hands, and arms, and the friction of the rapidly moving muscle tendons inside the tunnel results in swelling and compression of the nerve. So, can CTS really be prevented?
There are many factors associated with CTS, and some risks can be prevented. For example, some conditions like diabetes, rheumatoid arthritis, and IBS increase the risk of CTS. Therefore, it would be safe to assume those who better manage such conditions would have a lower risk for developing CTS.
Due to the many factors associated with CTS, there is no “one size fits all” when it comes to treatment and prevention of CTS. With that said, here are some VERY effective methods:
1) Ergonomic workstation modifications: Altering the work space (monitor height, keyboard/mouse style, different chair, chair/desk height, etc.) to reduce the number and speed of movements needed to perform commons work tasks.
2) Rest periods: Insert “micro-breaks” into a busy task. Combine breaks with stretching exercises of the wrist/hand/fingers and vary job tasks between fast and slow repetitive types.
3) Exercise: Shake the fingers and hands, lean back in a chair with the arms/shoulders stretched back (“Brugger’s Exercise”), move the neck (chin tucks, rotations, etc.), bend the hand/wrist backwards on a wall or the desk’s edge, self-massage and deep tissue release of the forearm and hand muscles. Do regular aerobic exercise (walking, swimming, biking, etc.) several times each week.
4) Posture: Sit up straight, elbows about 90° on height-adjustable arm rests or comfortably at the sides, forearms parallel to the floor; knees level or slightly lower than the hips, feet flat on the floor or on a footrest or box, if needed. Place typing materials at eye level / avoid prolonged head/neck rotation. Use a wrist rest for the keyboard and mouse, and use a headset when on the phone.
5) Reduce hand tool forces: Choose a tool that allows the wrist to remain neutral. Avoid side to side and flexion/extension wrist positions—especially if they’re prolonged! Tool handles should NOT dig into the palm of the hand or the wrist, and should not have sharp edges. A textured handle can improve grip. Minimize vibration from power tools. Wear shock absorbing gloves. Avoid cold work environments and cold tools.
6) Diet: Cut down on caffeine and smoking. Avoid obesity—a known risk factor of CTS! Consider an anti-inflammatory diet (Paleo, Mediterranean).
7) Splints: A wrist cock-up splint at night prevents prolonged faulty positions and REALLY helps!
This is a partial list of preventative measures that can REALLY help. Doctors of chiropractic treat the WHOLE person and can teach you the right exercises, ways to modify your diet, offer manual therapies and modalities, and help guide you in your self-management of CTS, as this can be a lifelong affliction. A multi-modal treatment approach generally works best!
Is Surgery Always Required?
Carpal tunnel syndrome (CTS) is the most common peripheral entrapment neuropathy—that is, it’s the most common place to trap a nerve in the extremities (arms or legs). CTS affects 6-11% of adults in the general population, and it occurs in women more often than men. The cause is often difficult to determine but the most common reasons can include trauma, repetitive maneuvers, certain diseases, pregnancy, being over the age of 50, and obesity.
So, is surgery the only answer? The short answer is NO! In fact, in a recent randomized clinical trial published in the Journal of Pain, researchers observed similar improvements in function when they compared the outcomes of patients who underwent surgery vs. those who received manual therapies (such as those performed several times a day at chiropractic clinics around the world) at both six months and one year later. The improvements included increased strength, function, and decreased hypersensitivity in both the surgical and non-surgical groups. Interestingly, the manual therapy group did BETTER at the one and three month assessments when compared with the surgical group (again, with no difference at six and twelve months)!
The median nerve, the culprit behind CTS, starts in the neck and travels down through the shoulder, elbow, forearm, and finally through the carpal tunnel, which is made up of eight small carpal bones that form the arch of the bridge. Entrapment of the median nerve occurs when the normally tight quarters within the carpal tunnel combine with the inflamed nine sheathed muscle tendons that push the nerve into the floor of the tunnel (a ligament), which results in CTS! The goal of therapy—both surgical and manual therapy—is to reduce the pressure within the tunnel and free up the compression of the median nerve.
Manual therapies focus on joint mobilization and manipulation to reduce joint fixations, muscle release techniques in the forearm and hand, stretching techniques, and at-home exercises that emphasize a similar stretch, the night brace, and management of any underlying contributing factor. These “underlying factors” might include diabetes, hypothyroid, taking birth control pills, weight management, and inflammatory arthritis.

CTS at Night.
For those who have carpal tunnel syndrome (CTS), it’s no surprise that CTS is frequently most expressive during the night, often to the point of interrupting sleep and/or making it difficult to fall back to sleep. So why is that?
The primary reason for nighttime CTS symptoms has to do with the wrist, as it is very difficult to sleep with the wrist held in its “ideal” or least irritating position. In fact, most people favor “curling” the back of the hand under the chin or bending the hand/wrist backwards under the head. When the wrist is bent in either direction, it can increase the pressure inside the wrist, which can generate the various symptoms associated with CTS.
One study evaluated the pressure inside the carpal tunnel while participants slowly moved their wrists. The researchers found many movements didn’t need to exceed 20 degrees before the pressure increased enough within the carpal tunnel to generate symptoms.
Because it doesn’t take a lot of movement to build up excessive pressure in the wrists of those with CTS, many doctors recommend the use of a “cock-up splint” for the non-surgical treatment of CTS in order to help keep the wrist in a neutral position.
Wrist posture is also an important factor during the day. One study looked at typing on a tablet PC, which allowed people to work in non-traditional settings. As screen size reduced, the posture required to type became more limited and accelerated the usual rate of pain onset in the neck, elbows, and wrists.
This study also looked at three different positions used when working on touch-screen devices: desk, lap, and bed. The healthy subjects completed six, 60-minute typing sessions using three virtual keyboard designs: standard, wide, and split. The researchers monitored the position of the wrist, elbow, and neck while the participants typed and followed up each session with questionnaires designed to measure discomfort.
The research team reported that typing in bed required greater wrist extension but resulted in a more natural elbow position than typing at a desk. The angled split keyboard significantly reduced the wrist deviation vs. the standard or wide keyboard designs. All three regions—the neck, elbow, and wrist—exhibited more movements (13% to 38%) towards the end of the one hour sessions, which correlated with a significant increase in pain in every body region investigated. Overall, using a wider keyboard while sitting at a desk was the most tolerable position among study participants.