Your cubital tunnel is the groove on the inside of your elbow, also called the “funny bone.” The funny part about the funny bone is that it is not actually a bone but rather a nerve, called the ulnar nerve. Your ulnar nerve begins in your neck and passes through the cubital tunnel on its way to your hand.
 When you flex your elbow, the ulnar nerve is required to both stretch and slide through your cubital tunnel. If your ulnar nerve is “stuck” in the tunnel and does not glide when you flex your elbow, this leads to traction and irritation of the nerve. This is called “cubital tunnel syndrome.” The nerve may also be irritated from direct compression, like leaning your elbow on the edge of a desk or from arthritic spurs. Cubital tunnel syndrome is the second most common nerve compression problem in the arm, behind carpal tunnel syndrome.
When you flex your elbow, the ulnar nerve is required to both stretch and slide through your cubital tunnel. If your ulnar nerve is “stuck” in the tunnel and does not glide when you flex your elbow, this leads to traction and irritation of the nerve. This is called “cubital tunnel syndrome.” The nerve may also be irritated from direct compression, like leaning your elbow on the edge of a desk or from arthritic spurs. Cubital tunnel syndrome is the second most common nerve compression problem in the arm, behind carpal tunnel syndrome.
Irritation of the ulnar nerve in the cubital tunnel causes pain, numbness or tingling that radiates from your elbow into your fourth and fifth fingers. Your symptoms can vary from a vague increased sensitivity to pain. The symptoms are common at night and are often progressive over time. In severe cases, you may begin to lose grip strength and fine muscle control.
Cubital tunnel syndrome is commonly seen in baseball, tennis and racquetball players. Workers who keep their elbows flexed such as holding a tool or telephone, or those who press the ulnar nerve against a hard surface like a desk, are at an increased risk for this disorder. Cubital tunnel syndrome affects men three to eight times as often as women and is more common in those who have diabetes or are overweight.
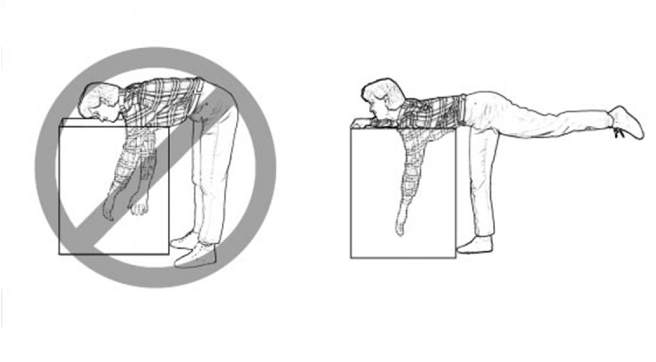
You should try to avoid prolonged elbow flexion or direct pressure over your elbow. Our office may prescribe a nighttime elbow splint that limits flexion.