The temporalis muscle is located in the temple area of the skull. It originates on the temporal lines on the parietal bone of the skull, and inserts on the coronoid process of the mandible. It’s main action is to close the jaw. The posterior and middle fibres bilaterally retrude the mandible. Acting individually, this muscle will deviate the mandible to the same side. Trigger points in this muscle refer into the teeth causing hypersensitivity, and into and above the eye and temple, causing headaches.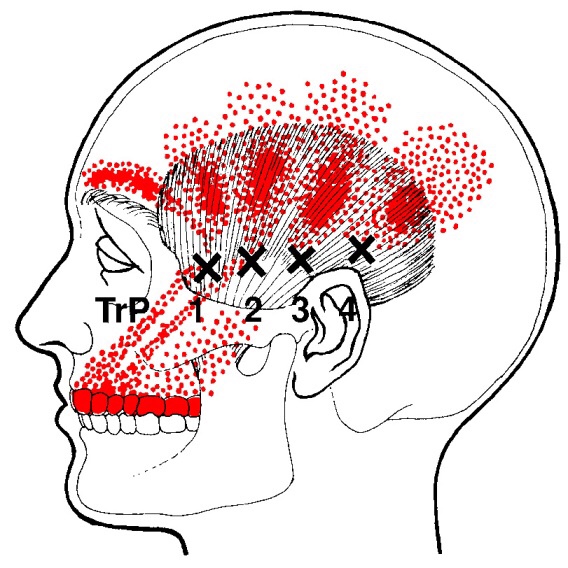
Posture
Do you wake up with numb fingers?
The term “thoracic outlet” describes an area at the base of your neck, just above your collarbone. Some important nerves and vessels pass through this outlet on their way into your arm. Compression of these tissues causes a condition called “thoracic outlet syndrome” which results in pain, numbness or tingling in your arm.
Several different factors can cause Thoracic Outlet Syndrome,

commonly referred to as TOS. Sometimes TOS is caused from tightness in the muscles of your neck and chest, other times the space between your first rib and collarbone is too small. People who have an extra rib (cervical rib) and people who have recently suffered a neck injury may have a greater chance of having this problem.
The condition is aggravated by poor posture and by occupations that promote “slouching,” i.e., computer users, assembly line workers, supermarket checkers and students. Swimmers, volleyball players, tennis players, baseball pitchers and occupations requiring prolonged overhead activity. i.e., electricians and painters are also prime candidates for TOS.
Symptoms of TOS include arm pain, numbness, tingling and possible weakness. Neck, arm and hand pain may begin slowly and are often aggravated by elevation of the arms or excessive head movement. Loss of grip strength is possible.
Conservative treatment, like the kind we provide, has been shown to be effective at treating TOS. Through our careful exam we have identified your specific sites of compression and will use some of the following treatment to help:
You should avoid carrying heavy loads, especially on your shoulder i.e., carpet rolls. Briefcases, laptop cases or heavy shoulder bags should be lightened. Bra straps may need additional padding or consideration of replacement with a sports bra.
Trigger points in the lateral pterygoid
The lateral pterygoid muscle plays an important role in prober jaw function. It originates on the greater wing of the sphenoid bone and the lateral pterygoid plate, and inserts on the condyloid process of the mandible. It’s action is to pull the head of the mandibular condyle out of the mandibular fossa while opening the jaw. When trigger points develop they refer pain into the temporal mandibular joint and maxillary sinus. This referral is commonly mistaken for TM arthritis. In addition to the referral pain, trigger points in this muscle can also effect proper movement of the jaw.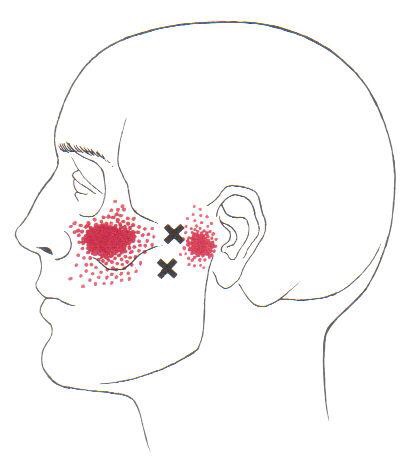

Trigger points in the serratus anterior
The serratus anterior muscle is located along the sides of the ribs. It originates on the outer surface of the upper 8-9ribs, and inserts on the medial border of the scapula. This muscle acts on the scapula in several different ways. First it rotates the scapula to turn the glenoid fossa upward. It also protracted and elevates the scapula. And lastly it helps to prevent wining. This muscle is often shortened from prolonged sitting and work on a computer. Active trigger points in this muscle refer pain locally around the trigger point with spillover down the inside of the arm. Pain can also radiate into the inferior angle of the scapula. 
There is nothing great about greater trochanteric pain syndrome. Nothing at all.
Your hip typically has about six small fluid-filled sacs called “bursa” that act as cushions between tendons and bone. One of the most common causes of hip pain is a condition called, “hip bursitis” which means that one or more of your bursas have become painfully inflamed. The broader (more accurate) diagnosis of “Greater trochanteric pain syndrome” (GTPS) describes an uncomfortable collection of problems affecting the outermost portion of your hip. GTPS can include swelling of one or more of the fibrous tendons that attach your muscles onto your hip – a condition called, “tendinitis.” In addition to bursitis & tendonitis, GTPS may originate from tightness in the muscle that travels over your hip en route to your knee- resulting in compression and irritation to your hip.

Greater trochanteric pain syndrome is most common in middle age to elderly adults and is 2-4 times more common in females. Sometimes the problem affects both hips at the same time. Approximately 1/3 of patients with GTPS have lower back pain. Patients who have arthritis in their hips and knees are more likely to suffer from ongoing complaints.
Your symptoms probably include a persistent pain on the outside of your hip, buttock, and upper thigh. Your discomfort may be aggravated by sitting with your leg crossed, arising from a seated position, prolonged standing, climbing stairs, and high-impact activities, like running. Sometimes patients find it difficult to sleep, since lying on the painful hip usually increases symptoms.
For adults, x-rays may or may not be needed to confirm the diagnosis, but children and adolescents usually require films to rule out more serious childhood diseases. Be sure to tell your doctor if you notice that you have a fever, leg numbness, pain radiating significantly beyond your knee, or pain in the front of your groin crease (the area where you leg meets your pelvis.)
Conservative treatment, like the type provided in this office, is successful in about 90% of cases. If you have acute pain, you may need to temporarily limit or discontinue activities that increase your discomfort. Using ice or ice massage at home may help. Some patients find temporarily relief by applying sports creams. Very commonly, patients with pain on the outside of their hip suffer from weakness in one of their buttock muscles, called the “gluteus medius.” When this muscle lacks strength, it is unable to protect your hip during normal activities, like walking. Research has shown that strengthening your hip has a dramatic effect on your progress.
Athletes should avoid running on a banked surface, like the crown of a road or indoor track. Be sure to reverse directions each mile if you run on a circular track. Avoid running on wet or icy surfaces, as this can cause increased tension in your hip. Runners with a “lazy” narrow-based running gait will benefit by increasing their step width to minimize stress on their hip. Cyclists need to make sure that their seat is not positioned too high. Overweight patients should consider weight reduction programs.
I have Plantar Fasciitis; now what?
The “Plantar fascia” is a fibrous band running from the under surface of your heel to the ball of your foot. “Plantar fasciitis” is a painful inflammation of this tissue caused by chronic over stretching and mild tearing.
Plantar fasciitis is commonly associated with fallen arches of the foot. To understand how this happens, cup your hand to make a “C” shape. This represents a foot with a high arch. Imagine a band running from your fingertips to your wrist. This represents the plantar fascia. Now, straighten your fingers to simulate what happens when the arch “falls.” When this happens in your foot, the plantar fascia is stretched and can begin to tear away from your heel.

Plantar fasciitis affects 10% of the population and is more common in women. Approximately one fourth of patients have the problem in both feet at the same time. People who place excessive stress on their feet by being overweight, standing for long periods, or participating in endurance sports are more likely to develop the condition as well. Shoes without adequate arch supports, including sandals or going barefoot, increase your chances of developing plantar fasciitis. Wearing high-heeled shoes or boots may contribute to the problem.
The most common symptom of plantar fasciitis is pain in the heel or arch when standing up after a period of inactivity, particularly first thing in the morning. When you are sleeping, the arch is in a relaxed or shortened state, and the plantar fascia is able to heal. When you stand up first thing in the morning, you stretch the fascia, once again tearing it away from its attachment on the heel. The condition may progress to the point that you experience pain throughout the day, even while resting. The pain often eases after you walk for a period of time, only to redevelop. You may notice some tenderness when you touch your heel, and you probably have tight calf and hamstring muscles as well.
Plantar fasciitis can be a frustrating condition, often lasting 18 months or more if left untreated. Fortunately, you may recover more quickly with proper treatment. One of the most important things that you can do is to make sure that you are wearing shoes with good arch supports on a consistent basis. A period of rest may be necessary to help you recover. Runners may need to temporarily decrease mileage or switch to less stressful activities like swimming, cycling, or using an elliptical machine. A splint or “Strassburg sock” worn at night will help to keep your plantar fascia in a stretched position while it is healing.
Trigger points in the iliopsoas muscle
This muscle originates on the bodies and disks of T12-L5 and the inner ilium. It inserts on the lesser trochanter of the femur. The psoas flexes the hip when the spine is fixed. When the leg is fixed it extends the lumbar spine increasing lumbar lordosis. This Muscle is often chronically shortened due to inactivity and sitting posture. When trigger points are present they will refer pain primarily to the lower lumbar area and the sacrum as well as into the anterior thigh. Trigger points in the iliopsoas muscle can mimic appendicitis.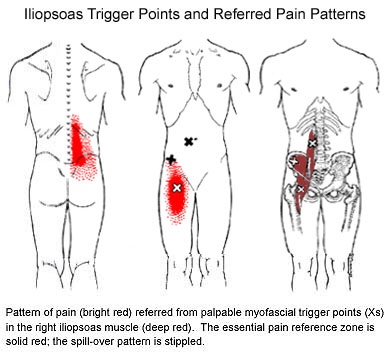
Exercise of the Month: Dead Bug
Dead Bug
Begin lying on your back with your right arm reaching overhead and your left leg flat on the table. Your right knee should be bent 90 degrees and your hip 45 degrees. Place your left wrist beneath your back to prevent your back from flattening against the ground. Slowly begin by raising your left knee and right arm at the same time until your hand touches your knee. Be sure not to lift your head or allow your spine to flatten against the floor. Return to the start position and repeat for three sets of 10 repetitions on each side, twice per day or as directed.
My abductors are weak, what does that mean?

Weakness of the gluteus medius allows your pelvis to drop and your knee to dive inward when you walk or run. This places tremendous strain on your hip and knee and may cause other problems too. When your knee dives inward, your kneecap is forced outward, causing it to rub harder against your thigh bone- creating a painful irritation and eventually arthritis. Walking and running with a relative “knock knee” position places tremendous stress on the ligaments around your knee and is a known cause of “sprains”. Downstream, a “knock knee” position puts additional stress on the arch of your foot, leading to other painful problems, like plantar fasciitis. Upstream, weak hips allow your pelvis to roll forward which forces your spine into a “sway back” posture. This is a known cause of lower back pain. Hip muscle weakness seems to be more common in females, especially athletes.
You should avoid activities that cause prolonged stretching of the hip abductors, like “hanging on one hip” while standing, sitting crossed legged, and sleeping in a side-lying position with your top knee flexed and touching the bed. Patients with fallen arches may benefit from arch supports or orthotics. Obesity causes more stress to the hip muscles, so overweight patients may benefit from a diet and exercise program. The most important treatment for hip abductor weakness is strength training. Hip strengthening is directly linked to symptom improvement. Moreover, people with stronger hip muscles are less likely to become injured in the first place. The exercises listed below are critical for your recovery.
Meet the Hip Cycle. You can thank me later.
1. Side lying with back and shoulders against a wall so you can’t roll back.
2. Bend your bottom leg and put the sole of your foot against the wall to be more stable.
3. Start position is with your foot directly in line with your hip. Do not let it get any lower than that. The highest point of your foot needs to be the bump on the outside of your ankle.
Do 5-10 reps of each of the following without rest between exercises twice a day. The goal is 20 reps each.
a. 6″ leg raises in abduction
b. Knee up to chest (90* knee and hip)
c. 12″ leg raises into abduction
d. Bicycling (knee up to chest, extend knee and sweep back to start with leg straight)
e. Clockwise circles
f. Counterclockwise circles
Good luck.
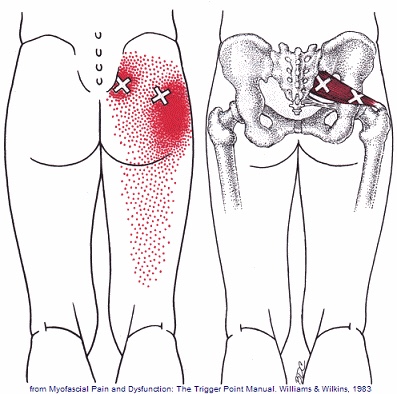
Trigger points in the piriformis muscle
The piriformis muscle is a small muscle deep to glute max and lies over top of the sciatic nerve. It originates on the anterior sacrum, and inserts on the greater trochanter of the femur. It’s main action is to laterally rotate the femur. When trigger points developed in this muscle they will refer pain into the sacro-iliac region, across the posterior hip and down the leg. This muscle can also be a cause of sciatic nerve irritation if it gets tight, causing “sciatica” symptoms.