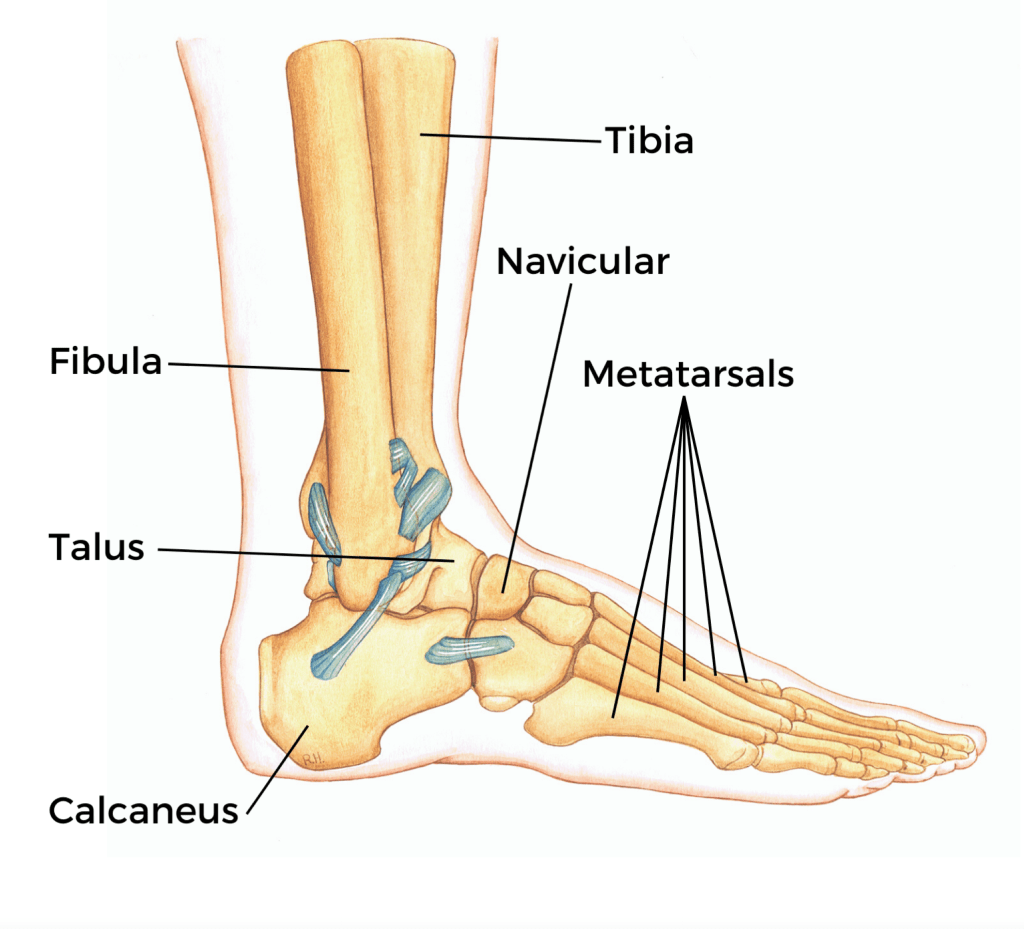
Meralgia paresthetica is often an overlooked diagnosis for symptoms such as tingling, numbness, and burning pain on the front and outside of the thigh. This condition results from the compression or irritation of the lateral femoral cutaneous nerve, which supplies sensation to the thigh.
Causes and Risk Factors
The lateral femoral cutaneous nerve can become compressed beneath a ligament, tendon, or tight muscle in the hip and pelvis. Several factors can increase the likelihood of developing meralgia paresthetica, including:
- Pregnancy: The added weight and changes in body mechanics during pregnancy can increase pressure on the nerve.
- Excess Weight: Being even slightly overweight can exacerbate nerve compression.
- Tight Clothing: Items such as girdles, compressive shorts, or tight belts can aggravate the condition.
- Occupational Equipment: Carpenters’ tool belts or police duty belts may compress the nerve.
- Prolonged Positions: Sitting for extended periods or lying in a fetal position can worsen symptoms.
- Diabetes: Diabetics are at greater risk due to the potential for nerve damage associated with the condition.
Symptoms
In the early stages, symptoms of meralgia paresthetica are usually mild and intermittent. Walking or standing can aggravate the symptoms, while sitting tends to provide relief. As the condition progresses, numbness and tingling can develop into severe, shooting pain that may not be alleviated by changing positions.
Chiropractic Care: A Non-Invasive Solution
Chiropractic care offers a holistic, non-invasive approach to managing and treating meralgia paresthetica. Here’s how chiropractic can help:
1. Spinal and Pelvic Adjustments
Chiropractors perform adjustments to correct any misalignments in the spine and pelvis that may contribute to nerve compression. These adjustments help restore proper alignment and reduce pressure on the lateral femoral cutaneous nerve.
2. Soft Tissue Therapy
Techniques such as massage, myofascial release, and trigger point therapy can alleviate muscle tightness and tension in the hip and pelvis area, which can help reduce nerve compression.
3. Stretching and Strengthening Exercises
Chiropractors provide personalized exercise programs to stretch tight muscles and strengthen weak ones. These exercises can improve flexibility and stability in the hip and pelvis, further reducing pressure on the nerve.
4. Posture and Ergonomic Advice
Poor posture and improper ergonomics can contribute to nerve compression. Chiropractors can offer guidance on maintaining proper posture and making ergonomic adjustments at work or home to prevent aggravating the condition.
5. Lifestyle Modifications
Chiropractors can recommend lifestyle changes to help manage symptoms. This might include weight management strategies to reduce excess tissue compression, advice on wearing looser clothing, and alternative solutions for occupational equipment that doesn’t place pressure on the affected area.
Practical Tips for Managing Meralgia Paresthetica
- Wear Looser Clothing: Avoid tight belts, girdles, or compressive shorts. Opt for suspenders instead of a belt if necessary.
- Adjust Occupational Equipment: If you use a tool belt or duty belt, ensure it doesn’t place excessive pressure on the hip area.
- Maintain a Healthy Weight: A sensible weight loss program can help reduce compression from excess tissue.
- Modify Your Posture: Avoid prolonged sitting or lying in positions that aggravate your symptoms.
- Engage in Regular Exercise: Incorporate stretching and strengthening exercises into your routine to maintain muscle balance and reduce nerve compression.
Conclusion
Meralgia paresthetica can significantly impact your quality of life, but with the right approach, you can manage and alleviate your symptoms. Chiropractic care provides a comprehensive, non-invasive treatment option that addresses the root causes of nerve compression. At River East Chiropractic, our new facility offers a range of services, including chiropractic, acupuncture, massage, occupational therapy, and a full gym to support your recovery and overall well-being.
Contact us today to schedule an appointment and start your journey toward relief from meralgia paresthetica. Follow us on social media for more health tips and updates on how chiropractic care can improve your quality of life.