The quadratus lumborum muscle is a commonly overlooked source of low back pain and is often responsible for “pseudo disc syndrome”. This muscle originates on the inferior border of the 12th rib and lumbar transverse processes. It inserts on the iliac crest and iliolumbar ligament. The q.l.’s main actions are extension and lateral flexion of the spine. It also acts as a stabilizer of the lumbar spine. Trigger points in this muscle refer pain into the sacroiliac joint and the lower buttock. Pain can also spread anteriorly along the crest of the ilium into the lower abdomen and groin and to the greater trochanter. 
Hip Pain
Want a fancy new hip? Start with this!
A “joint” is an area where two or more bones come together. These bones have a slick rubbery protective covering, called “cartilage,” on the areas where they meet. This cartilage serves as a friction reducer and shock absorber, thereby prolonging the health of our joints.
Osteoarthritis, or simply arthritis, occurs when your joint cartilage degenerates as a result of repetitive stress.

Over time, this cartilage can thin and crack, eventually wearing away, leading to a painful “bone on bone” situation. Thinning of your joint cartilage is often accompanied by the development of “bone spurs” and/or joint deformity further disrupting your joint function.
Hip arthritis is common, affecting up to one-third of the population. The likelihood of you developing osteoarthritis increases as you age, and appears to be at least partially inherited from your parents. It is more common if you have been overweight and if you were subjected to repetitive injury, including occupations & sports requiring prolonged standing or heavy physical exertion.
An early symptom of Hip OA is prolonged stiffness upon arising in the morning and following periods of inactivity. You might complain of the inability to put your socks on, shave your legs or climb stairs. Groin, thigh and buttock pain are common. In some cases the pain can radiate into your lower leg. Cracking and popping of your hip when moving is possible.
It is sometimes difficult for doctors to differentiate between hip osteoarthritis and lower back problems that can also cause hip pain. Your doctor will likely X-ray your hip to determine the extent of your arthritis (graded 1-4 based on severity).
Arthritis cannot be cured, but your symptoms can often be relieved. Treatment of hip arthritis may include exercises, especially water-based programs like “water-aerobics.” Your doctor may use physical therapy modalities and will likely stretch and manipulate your hip, as this has been shown to be effective at relieving symptoms.
Your doctor may recommend that you avoid aggravating activities, especially those requiring you to rotate your hip internally (i.e., pigeon toed” movements), and to maintain a healthy weight. You will be taught home stretching and strengthening exercises to help you recover. Taking 1500 mg of Glucosamine and chondroitin has been shown to help some arthritis sufferers.
In more severe cases, you may need to use a cane (in the opposite hand) to take weight off the arthritic hip. If conservative treatment fails to relieve your pain, your doctor might recommend consultation with an orthopedic hip specialist to consider joint replacement.
I’ve got ITB Syndrome Doc! Now What?
Your iliotibial band is a fibrous band of tissue running from the crest of your hip, down to your knee. A muscle near the crest of your hip called the tensor fascia lata, attaches to this band to help control movements of your leg. Your iliotibial band passes over the point of your hip and over another bony bump on the outside of your knee called the lateral epicondyle. When the band is too tight, it can become painfully inflamed as it repeatedly rubs over the top of either of these bony projections. Irritation at the bony bump near the knee is called iliotibial band friction syndrome.

The condition usually presents as pain on the outside of your knee that becomes worse with repetitive knee flexion or extension. This condition is the leading cause of lateral knee pain in runners, especially slower “joggers.” The pain usually develops 10-15 minutes into the workout. You may sometimes feel or hear a click during movement. Symptoms generally ease at rest. Running on slick “wintry” surfaces may aggravate the condition. Excessively worn running shoes may be a culprit.
This problem is commonly caused by weakness in your gluteal muscles. When these muscles are weak, the muscle that attaches to your iliotibial band must contract harder to stabilize your hip. Having one leg longer than another is a known aggravating factor.
Runners should minimize downhill running and avoid running on a banked surface like the crown of a road or indoor track, as well as wet or icy surfaces. Runners should reverse directions on a circular track at least each mile. Bicyclists may need to adjust seat height and avoid “toe in” pedal positions. Avoid using stair climbers or performing squats and dead lifts. Sports cream and home ice massage may provide some relief of symptoms.
The all too common knee cartilage tear.
The meniscus is a piece of tough, smooth, rubbery cartilage in the middle of your knee. Each of your knees have a meniscus on the inside (medial meniscus) and another on the outside (lateral meniscus). Each meniscus attaches to the top of your shin bone (tibia) and acts as a shock absorbent guide for your thigh bone (femur), which rests above.

Symptoms of meniscus injury depend on the type and severity of damage. Patients sometimes hear a pop or snap at the time of initial injury. Patients with acute injuries may have difficulty bearing weight and may develop a limp. Stiffness is a common complaint. Clicking, catching, locking or giving-way is possible. Meniscus injuries are usually aggravated by movement and become particularly uncomfortable with deep squatting.
Although some meniscus injuries may require surgery, most can be treated conservatively with the type of treatments provided in our office. Your age roughly correlates with the need for surgery. Approximately 2/3 of acute meniscal tears in children and adolescents will require surgery, but only about 1 in 20 patients over the age of 40 will require knee arthroscopy. Surgery is necessary more often in patients who cannot fully bend or straighten their leg, or whose knee locks and gets stuck in one place.
Home management includes rest, ice, compression and elevation (RICE). You should apply ice over your knee for 15 minutes at a time, three or four times a day. Wrapping an ACE bandage around your knee will provide compression to help minimize swelling. You may elevate your leg by placing a pillow beneath your knee to help reduce swelling.
You may need to limit your activity to prevent further damage while you are recovering from injury. Activities that involve twisting on a weight-bearing flexed knee are the most harmful. You may need to temporarily or permanently discontinue some high energy sports activity. Other activities, like water walking, may be substituted for higher energy sports, like soccer and tennis. Ice or ice massage should be used following activity.
Patients who have undergone surgical repair of their meniscus are more likely to develop arthritis. These patients will also benefit from a well-planned home exercise program.
FAI starts you on the road to failure.
Your hip socket or “acetabulum” is covered by smooth, glassy cartilage extending all the way to its outer rim. The term “Femoroacetabular impingement” (FAI) means that this rim of cartilage is being pinched when you move your hip into certain positions. Repetitive pinching results in irritation, tearing, or even detachment of this cartilage from your hip socket.

FAI occurs because of a mismatch between the head of your femur and the socket of your hip. The mismatch may be from an abnormally shaped hip bone (cam deformity), or having too much cartilage on the rim of your hip socket (pincer deformity). Most frequently, FAI results from a combination of both (combined or mixed deformity).
FAI is most common in young active people. Although the deformity may be present on both sides, symptoms are usually one-sided. The condition is equally common among men and women. Symptoms of FAI include a constant dull pain with periods of sharp pain, made worse by activity. Walking, pivoting, prolonged sitting, stair climbing, and impact activities like running or jumping can aggravate your symptoms. Snapping, locking, and clicking are common.
Our office will help direct a rehab program to maximize your chance of recovery. You should attempt to stay active, but avoid activities that aggravate symptoms. You may consider temporarily switching to low-impact activities, like stationary biking or water-walking. You should avoid motions that combine flexion and internal rotation, like- getting out of a car with one leg at a time, swimming the breaststroke, or performing squats. Patients with FAI should avoid excessive stretching, as this could aggravate the condition, but will likely benefit from strengthening exercises in the type of treatment provided in this office.
There is nothing great about greater trochanteric pain syndrome. Nothing at all.
Your hip typically has about six small fluid-filled sacs called “bursa” that act as cushions between tendons and bone. One of the most common causes of hip pain is a condition called, “hip bursitis” which means that one or more of your bursas have become painfully inflamed. The broader (more accurate) diagnosis of “Greater trochanteric pain syndrome” (GTPS) describes an uncomfortable collection of problems affecting the outermost portion of your hip. GTPS can include swelling of one or more of the fibrous tendons that attach your muscles onto your hip – a condition called, “tendinitis.” In addition to bursitis & tendonitis, GTPS may originate from tightness in the muscle that travels over your hip en route to your knee- resulting in compression and irritation to your hip.

Greater trochanteric pain syndrome is most common in middle age to elderly adults and is 2-4 times more common in females. Sometimes the problem affects both hips at the same time. Approximately 1/3 of patients with GTPS have lower back pain. Patients who have arthritis in their hips and knees are more likely to suffer from ongoing complaints.
Your symptoms probably include a persistent pain on the outside of your hip, buttock, and upper thigh. Your discomfort may be aggravated by sitting with your leg crossed, arising from a seated position, prolonged standing, climbing stairs, and high-impact activities, like running. Sometimes patients find it difficult to sleep, since lying on the painful hip usually increases symptoms.
For adults, x-rays may or may not be needed to confirm the diagnosis, but children and adolescents usually require films to rule out more serious childhood diseases. Be sure to tell your doctor if you notice that you have a fever, leg numbness, pain radiating significantly beyond your knee, or pain in the front of your groin crease (the area where you leg meets your pelvis.)
Conservative treatment, like the type provided in this office, is successful in about 90% of cases. If you have acute pain, you may need to temporarily limit or discontinue activities that increase your discomfort. Using ice or ice massage at home may help. Some patients find temporarily relief by applying sports creams. Very commonly, patients with pain on the outside of their hip suffer from weakness in one of their buttock muscles, called the “gluteus medius.” When this muscle lacks strength, it is unable to protect your hip during normal activities, like walking. Research has shown that strengthening your hip has a dramatic effect on your progress.
Athletes should avoid running on a banked surface, like the crown of a road or indoor track. Be sure to reverse directions each mile if you run on a circular track. Avoid running on wet or icy surfaces, as this can cause increased tension in your hip. Runners with a “lazy” narrow-based running gait will benefit by increasing their step width to minimize stress on their hip. Cyclists need to make sure that their seat is not positioned too high. Overweight patients should consider weight reduction programs.
Pes Anserine Bursitis; What Is It?
The term “pes anserine” is Latin for goose’s foot, and describes the appearance of three tendons that converge and insert on the inner portion of your knee. The pes anserine bursa is a fluid-filled, friction-reducing cushion, sandwiched between these tendons and your leg bone.
Injuries or irritation can cause the lining of the bursa to produce too much fluid, resulting in painful swelling. Patients with knee osteoarthritis are likely to have chronic irritation of the pes anserine bursa. The condition is more common in overweight patients, diabetics, and females. Runners and athletes in sports that require rapid side-to-side movements (i.e. football, soccer, tennis, etc.) are more likely suffer from the condition. Swimmers who do the breast stroke commonly suffer from pes anserine bursitis.
 Symptoms include pain on the inner side of your knee, just below the joint. Your pain is probably worse when you stand up or walk stairs. Discomfort increases during activities that require side-to-side movements (i.e. tennis, dancing). Be sure to tell your doctor if you notice clicking, popping, or locking of your knee, excessive thirst, excessive urination, fever, or pain & swelling in your calf.
Symptoms include pain on the inner side of your knee, just below the joint. Your pain is probably worse when you stand up or walk stairs. Discomfort increases during activities that require side-to-side movements (i.e. tennis, dancing). Be sure to tell your doctor if you notice clicking, popping, or locking of your knee, excessive thirst, excessive urination, fever, or pain & swelling in your calf.
In addition to the treatment provided by our office, you may find relief by applying home ice or ice massage for 8-10 minutes. Having flat feet places additional stress on the inside of your knee, so patients with fallen arches will benefit from arch supports or orthotics. Overweight patients will benefit from a diet and exercise program.
Trigger points in the iliopsoas muscle
This muscle originates on the bodies and disks of T12-L5 and the inner ilium. It inserts on the lesser trochanter of the femur. The psoas flexes the hip when the spine is fixed. When the leg is fixed it extends the lumbar spine increasing lumbar lordosis. This Muscle is often chronically shortened due to inactivity and sitting posture. When trigger points are present they will refer pain primarily to the lower lumbar area and the sacrum as well as into the anterior thigh. Trigger points in the iliopsoas muscle can mimic appendicitis.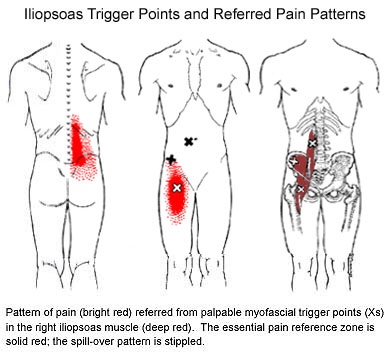
Pulled Hammie! Man Down!

Your hamstring is the group of muscles in the back of your thigh that flex your knee, i.e., moving your heel toward your buttock. The term “strain” means that a muscle or its tendon has been stressed beyond its limit and has frayed, much like a rope that has been pulled too hard. Your hamstring may be “pulled” or “strained” when it is forced to contract beyond its capacity, like during running or from excessive stretch. This tearing leads to bleeding, bruising, swelling, pain and loss of function.

The symptoms of a hamstring strain may vary from mild discomfort to severe pain, depending upon the amount of tissue that has been torn. Over 90% of hamstring strains occur abruptly with a tearing, burning or popping feeling accompanied by immediate pain below your buttock. Your symptoms will likely increase when straightening your leg, walking or flexing forward. You may notice some bruising that starts near the site of injury. Be sure to tell your doctor if you have notable pain in your lower back, if your pain extends into your calf, if your pain worsens with coughing or sneezing, or if you have a rash on the back of your thigh.
Hamstring injuries are more common when your muscles are tired from activity and happen more frequently as we age. Having excessive tightness or weakness in your hamstring, having quadriceps that are significantly stronger than your hamstring, having too little core strength or poor running form also predispose you to injury.
Nearly all hamstring strains can be successfully managed with conservative care, like the type provided in our office. Your healing period will vary based on several factors, including the specific region of your hamstring that has been injured. Tears that involve the part of the muscle closest to your ischial tuberosity (the bones you sit on) take longer to heal than those that occur further down the muscle.
Initially, you should use ice or ice massage over the injured area for 15 minutes at a time, up to once per hour. Our office may advise you to use an ACE wrap or compression bandage to help limit swelling. The use of NSAIDs for hamstring strains is controversial, as some research suggests this may delay healing. Patients who have more severe injuries may need to use crutches. While you are recovering, you may need to limit some activities, like running and jumping and instead, cross train by stationary cycling or swimming. You are more likely to strain your hamstring in the future and recurrent injuries may take twice as long to heal as the initial injury, so be sure to allow yourself adequate healing time, consistently perform your exercises and warm-up properly prior to activity.
My abductors are weak, what does that mean?

Weakness of the gluteus medius allows your pelvis to drop and your knee to dive inward when you walk or run. This places tremendous strain on your hip and knee and may cause other problems too. When your knee dives inward, your kneecap is forced outward, causing it to rub harder against your thigh bone- creating a painful irritation and eventually arthritis. Walking and running with a relative “knock knee” position places tremendous stress on the ligaments around your knee and is a known cause of “sprains”. Downstream, a “knock knee” position puts additional stress on the arch of your foot, leading to other painful problems, like plantar fasciitis. Upstream, weak hips allow your pelvis to roll forward which forces your spine into a “sway back” posture. This is a known cause of lower back pain. Hip muscle weakness seems to be more common in females, especially athletes.
You should avoid activities that cause prolonged stretching of the hip abductors, like “hanging on one hip” while standing, sitting crossed legged, and sleeping in a side-lying position with your top knee flexed and touching the bed. Patients with fallen arches may benefit from arch supports or orthotics. Obesity causes more stress to the hip muscles, so overweight patients may benefit from a diet and exercise program. The most important treatment for hip abductor weakness is strength training. Hip strengthening is directly linked to symptom improvement. Moreover, people with stronger hip muscles are less likely to become injured in the first place. The exercises listed below are critical for your recovery.
Meet the Hip Cycle. You can thank me later.
1. Side lying with back and shoulders against a wall so you can’t roll back.
2. Bend your bottom leg and put the sole of your foot against the wall to be more stable.
3. Start position is with your foot directly in line with your hip. Do not let it get any lower than that. The highest point of your foot needs to be the bump on the outside of your ankle.
Do 5-10 reps of each of the following without rest between exercises twice a day. The goal is 20 reps each.
a. 6″ leg raises in abduction
b. Knee up to chest (90* knee and hip)
c. 12″ leg raises into abduction
d. Bicycling (knee up to chest, extend knee and sweep back to start with leg straight)
e. Clockwise circles
f. Counterclockwise circles
Good luck.
