The adductor pollicis is a muscle in the hand and acts on the thumb. It originates on the transverse head of the third metacarpal, the oblique head of the base of the second and third metacarpals, and the trapezoid and capitate bones. It inserts on the base of the proximal phalanx and ulnar sesamoid. This muscle acts to adduct and flex the thumb. Trigger points cause pain and aching along the outside of the thumb and hand, spillover pain may reach the thenar eminence.
Hand Pain
Trigger points and fibromyalgia
Myofascial pain syndrome (trigger points) and fibromyalgia are often confused to be the same condition and while there is a lot of interrelatedness between the two they are not quite identical. The clinical definition of a trigger point is “a hyper irritable spot associated within a taut band of skeletal muscle that is painful on compression or muscle contraction, and usually responds with a referred pain pattern distant from the spot”. Trigger points form from an overload trauma to the muscle tissue. This is contrasted with fibromyalgia which is defined as “a medical condition characterized by chronic widespread pain and a heightened pain response to pressure. Other symptoms include tiredness to a degree that normal activities are affected, sleep problems and troubles with memory. Some people also report restless leg syndrome, bowel and bladder problems, numbness and tingling and sensitivity to noise, lights and temperature. It is also associated with depression, anxiety, and post traumatic stress disorder”. Fibromyalgia will also present with localized tender points which are often mistaken for trigger points. Where these two conditions become somewhat interrelated is via the nervous system. Fibromyalgia patients suffer from a super-sensitization of the nervous system causing hyperirritability and pain. Myofascial trigger points can be caused by,or be the cause of, super sensitization. An active trigger point will irritate the sensory nerves around it eventually leading to super-sensitization. Trigger points have also been showed to form of become active due to super-sensitization. Both of these conditions can perpetuate the other, leading to layers of pain and symptoms. This being the case, trigger point therapy can have a very positive effect on decreasing the severity of pain and symptoms in patients suffering from fibromyalgia.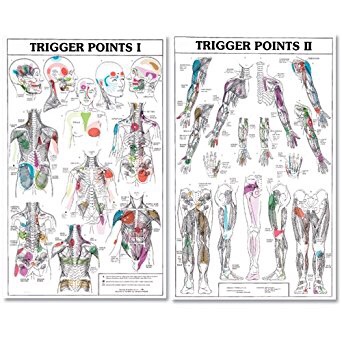

Bryan Cobb RMT.
Since 2005, Bryan has been dedicated to helping all people with chronic and acute pain caused by soft-tissue damage.
His training and experience make him uniquely qualified to treat a wide variety of pain and dysfunction and to give instruction on prevention and self-care.
Bryan is the only Massage Therapist in Manitoba — and one of the few in Canada — to be certified by the Certification Board for Myofascial Trigger Point Therapists (CBMTPT).
Bryan holds a degree as an Advanced Remedial Massage Therapist (ARMT) from the Massage Therapy College of Manitoba. Course work at MTCM includes
• over 2,000 hours of practice, as well as
• intensive course work,
• a supervised clinical practicum, and
• community outreach placements.MTCM has a credit transfer affiliation with the University of Winnipeg, ensuring that its courses are held to the highest level. When Bryan studied at MTCM, the college was the only massage therapy college in western Canada accredited by the Commission on Massage Therapy Accreditation. Today, the college is a member of the Canadian Council of Massage Therapy Schools.
Bryan is a member in good standing of the Natural Health Practitioners of Canada.
Bryan also has a background in Anatomy, Exercise Physiology, and Sport Sciences from the University of Manitoba, and he has worked as a personal trainer and fitness leader.
He is an avid natural bodybuilder and fitness enthusiast, and has a blue belt in Brazilian jiu-jitsu.
Osteoarthritis of the Hand
The bones in your hand have a slick, protective covering called “cartilage” on the joint surfaces that touch each other. This cartilage serves as a friction reducer and shock absorber, thereby, helping to extend the life of your joints. “Arthritis” means that your cartilage has begun to thin or crack and may eventually wear away –impairing your strength and dexterity. Painful hand arthritis affects

up to 1 in 4 people. This degeneration has a tendency to affect specific joints, especially those of your index and middle fingers and the base of your thumb.
Your chance of developing arthritis increases with age. Hand arthritis is 2 1/2 times more common in women. Arthritis occurs more often in joints that have been previously injured and in patients who perform repetitive movement of the hands- particularly labor and manufacturing jobs. Other risk factors include obesity and the presence of arthritis in your parents. Contrary to popular opinion, knuckle cracking does not increase your risk of arthritis, regardless of duration or frequency.
Symptoms usually begin slowly and progress into longstanding hand pain that comes and goes. Your symptoms are likely aggravated by activity and relieved by rest. Hard, bony enlargements often develop along the joint lines, especially in women. You may notice morning stiffness that subsides fairly quickly. Be sure to tell your doctor if you notice lasting morning stiffness or swelling, as this could be a sign of a different type of arthritis.
The American College of Rheumatology recommends the use of non-drug treatments (like the type provided in this office) for hand osteoarthritis. Patients with thumb osteoarthritis may benefit from a nighttime splint. Topical creams, especially those including “capsaicin” may help relieve symptoms. You may find relief by warming your hands with a hot pack or “paraffin bath” when they feel stiff. Some patients report benefit by taking Glucosamine Sulfate. The mainstay of treatment includes exercises to help improve your mobility and strength.
Pathophysiology of trigger points.
A large number of factors have been identified as causes of trigger point activation. These include acute or chronic overload of muscle tissue, disease, psychological distress, systemic inflammation, homeostatic imbalances, direct trauma, radiculopathy, infections, and lifestyle choices such as smoking. Trigger points form as a local contraction of muscle fibres in a muscle or bundle of muscle fibres. These can pull on ligaments and tendons associated with the muscle which can cause pain to be felt deep inside a joint. It is theorized that trigger points form from excessive release of acetylcholine causing sustained depolarization of muscle fibres. Trigger points present an abnormal biochemical composition with elevated levels of acetylcholine, noradrenaline and serotonin and a lower ph. The contracted fibres in a trigger point constricts blood supply to the area creating an energy crisis in the tissue that results in the production of sensitizing substances that interact with pain receptors producing pain. When trigger points are present in a muscle there is often pain and weakness in the associated structures. These pain patterns follow specific nerve pathways that have been well mapped to allow for accurate diagnosis or the causative pain factor.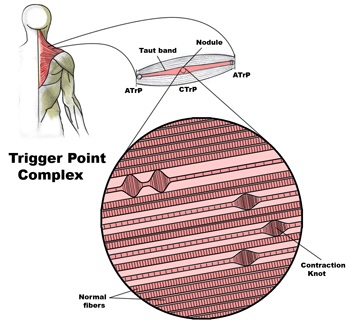
Diagnosis of trigger points.
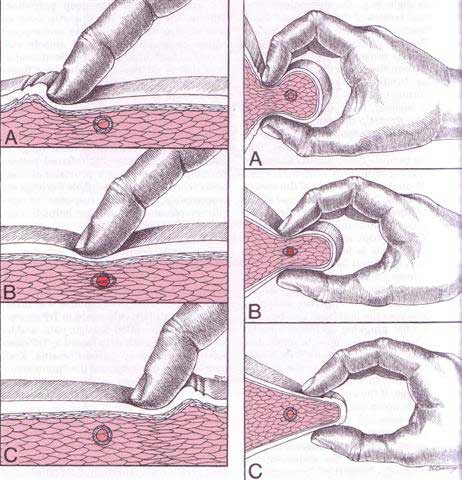
Diagnosis of trigger points typically takes into account symptoms, pain patterns, and manual palpation. When palpating the therapist will feel for a taut band of muscle with a hard nodule within it. Often a local twitch response will be elicited by running a finger perpendicular to the muscle fibres direction. Pressure applied to the trigger point will often reproduce the pain complaint of the patient and the referral pattern of the trigger point. Often there is a heat differential in the local area of the trigger point. 
What is a trigger point
Dr Janet travel coined the term trigger point in 1942 to describe clinical findings with characteristics of pain related a discrete irritable point in muscle or fascia that was not caused by acute trauma, inflammation, degeneration, neoplasm or infection. The painful point can be palpated as a nodule or tight band in the muscle that can produce a local twitch response when stimulated. Palpation of the trigger point reproduces the pain and symptoms of the patient and the pain radiates in a predictable referral pattern specific to the muscle harbouring the trigger point.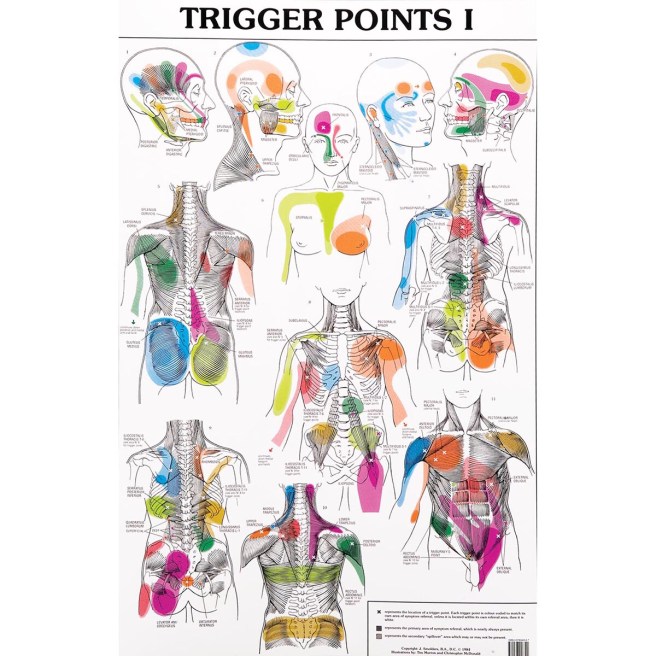
What to expect with a trigger point massage.
A treatment with Bryan is very user friendly. And, no, you don’t have to remove any clothing. However, bringing a t-shirt and a pair of shorts or sweats is recommended.
The first time you come for a treatment you will be asked to fill out a Client History form. Bryan will go over the information you provide, asking for more detail and discussing the type of pain you are having and its location.
The treatment itself involves locating the Trigger Points in the muscle or soft tissue and applying a deep focused pressure to the Point. This will reproduce the pain and the referral pattern that is characteristic of that pain.
The treatment will be uncomfortable at first, but as the Trigger Points release, the pain will decrease. The pressure will always be adjusted to your tolerance level. If, at any time, you feel too uncomfortable you can ask Bryan to ease off a bit.
Depending on your specific problem, Bryan may also use some stretching and / or range-of-motion techniques, as needed.
After treatment, it is usually recommended that the client apply moist heat to the area treated.
Another tunnel injury? Seriously?
Your radial nerve begins in your neck and travels past your elbow en route to its final destination in your hand. Just beyond your elbow, this nerve passes through a 2-inch area on the back of your forearm called the “Radial tunnel”. “Radial tunnel syndrome” means that your radial nerve has been compressed or irritated within this space-leading to forearm pain or hand weakness.

Radial tunnel syndrome is thought to result from muscular overuse, especially prolonged or excessive wrist extension or rotation. The most common cause of compression comes from excessive tightness in a muscle called the “Supinator”. Workers whose jobs require heavy or repetitive wrist movements are at an increased risk for this disorder. Occasionally, the radial nerve can become irritated from direct compression by a tight band or brace. The condition may be more common in those who have diabetes or thyroid problems.
Symptoms from irritation of the radial nerve depend upon which specific nerve fibers are irritated. The most common symptoms include pain, numbness, tingling or decreased sensitivity along the top of your forearm radiating toward your hand and thumb. The symptoms often mimic those of “tennis elbow.” When the nerve fibers that control muscle function become compressed, you may experience weakness when trying to extend your fingers, hand or wrist. Seventy percent of radial tunnel patients also have problems in their neck or upper back.
Conservative treatment of radial tunnel syndrome is generally successful. Fixing the problem means limiting excessive or repetitive wrist movements, especially extension and rotation. In severe cases, a splint may be necessary to limit your motion. Try to avoid compression of your forearm, particularly from tight bands or braces. Use of a tennis elbow brace will likely aggravate your symptoms. You may find relief by applying ice or ice massage to the area for 10-15 minutes at a time.
Cubital Tunnel Syndrome…. Ever heard of it?
Your cubital tunnel is the groove on the inside of your elbow, also called the “funny bone.” The funny part about the funny bone is that it is not actually a bone but rather a nerve, called the ulnar nerve. Your ulnar nerve begins in your neck and passes through the cubital tunnel on its way to your hand.
 When you flex your elbow, the ulnar nerve is required to both stretch and slide through your cubital tunnel. If your ulnar nerve is “stuck” in the tunnel and does not glide when you flex your elbow, this leads to traction and irritation of the nerve. This is called “cubital tunnel syndrome.” The nerve may also be irritated from direct compression, like leaning your elbow on the edge of a desk or from arthritic spurs. Cubital tunnel syndrome is the second most common nerve compression problem in the arm, behind carpal tunnel syndrome.
When you flex your elbow, the ulnar nerve is required to both stretch and slide through your cubital tunnel. If your ulnar nerve is “stuck” in the tunnel and does not glide when you flex your elbow, this leads to traction and irritation of the nerve. This is called “cubital tunnel syndrome.” The nerve may also be irritated from direct compression, like leaning your elbow on the edge of a desk or from arthritic spurs. Cubital tunnel syndrome is the second most common nerve compression problem in the arm, behind carpal tunnel syndrome.
Irritation of the ulnar nerve in the cubital tunnel causes pain, numbness or tingling that radiates from your elbow into your fourth and fifth fingers. Your symptoms can vary from a vague increased sensitivity to pain. The symptoms are common at night and are often progressive over time. In severe cases, you may begin to lose grip strength and fine muscle control.
Cubital tunnel syndrome is commonly seen in baseball, tennis and racquetball players. Workers who keep their elbows flexed such as holding a tool or telephone, or those who press the ulnar nerve against a hard surface like a desk, are at an increased risk for this disorder. Cubital tunnel syndrome affects men three to eight times as often as women and is more common in those who have diabetes or are overweight.
You should try to avoid prolonged elbow flexion or direct pressure over your elbow. Our office may prescribe a nighttime elbow splint that limits flexion.
