The trapezius muscle is a large diamond shaped muscle in your back and neck. It originates on the nuchal ligament and the spinous processes of c6-t12. It inserts on the scapular spine, acromion process, and the distal clavicle. It’s upper fibres act to elevate the shoulder and rotate the glenoid fossa upward. The lower fibres assist this motion. The middle fibres strongly adduct the scapula. This is the most common muscle in the human body to get trigger points. Trigger points in the lateral upper edge refer pain into the lateral neck and temples. Points in the mid and lower parts of the muscle refer pain into the posterior neck and shoulders. Trigger points in this muscle are a common cause of headaches.
fitness
Elbow pain and trigger points.
Did you know that tennis elbow and golfers elbow pain can be caused by trigger points? Points located in the forearm flexor and extensor muscles can cause pain, stiffness, and weakness in the elbow, forearm, wrist, and hand. Quite often these trigger point symptoms are mistaken for inflammation of the tendons which is what a true tennis/golfers elbow actually is. Failure to address the trigger points can lead to an incomplete recovery .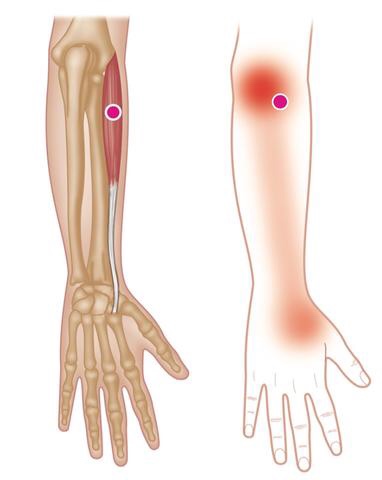
Trigger point massage
Session Description
A treatment with Bryan is very user friendly. And, no, you don’t have to remove any clothing. However, bringing a t-shirt and a pair of shorts or sweats is recommended.
The first time you come for a treatment you will be asked to fill out a Client History form. Bryan will go over the information you provide, asking for more detail and discussing the type of pain you are having and its location.
The treatment itself involves locating the Trigger Points in the muscle or soft tissue and applying a deep focused pressure to the Point. This will reproduce the pain and the referral pattern that is characteristic of that pain.
The treatment will be uncomfortable at first, but as the Trigger Points release, the pain will decrease. The pressure will always be adjusted to your tolerance level. If, at any time, you feel too uncomfortable you can ask Bryan to ease off a bit.
Depending on your specific problem, Bryan may also use some stretching and / or range-of-motion techniques, as needed.
After treatment, it is usually recommended that the client apply moist heat to the area treate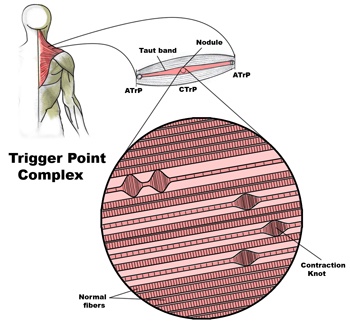
 d.
d.
Problems associated with trigger points
Trigger Points in muscle and other soft tissue are one of the most common causes of a wide variety of pain and dysfunction, including (but not limited to):
• Achy persistent pain
• Severe local pain
• Arm / leg pain
• Back pain
• Radiating pain
• Weakness
• Stiffness
• Pain resulting from a medical condition, such as
– Migraines
– Sciatica
– TMJ dysfunctions
– Arthritis
– Fibromyalgia
– Carpal tunnel syndrome
– Soft tissue injuries
– And more…
Trigger points in the levator scapula
The levator scapula is a muscle located in your neck. It originates on the transverse processes of C1-C4 vertebrae. It inserts on the superior part of the medial border of the scapula. This muscle acts to elevate the scapula and rotate the glenoid fossa downward. At the cervical attachment it acts to rotate the neck to the same side and assists extension. Trigger points will refer pain into the angle of the neck with spillover into the scapula. When this muscle is tight due to trigger points it will restrict neck rotation causing the classic stiff neck. With a forward head position this muscle often becomes stretched and over worked.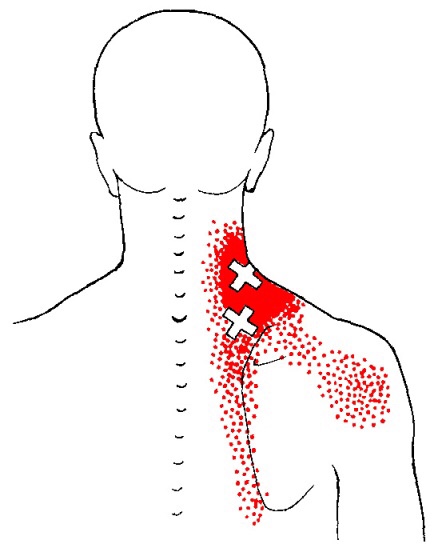
Trigger points in the lateral pterygoid muscle
The Lateral Pterygoid muscle is a muscle of the jaw. It originates on the greater wing of the sphenoid bone and the lateral pterygoid plate. It has its insertion on the condyloid process of the mandible. Functionally it it assists in opening the jaw by pulling the head of the mandibular condyle out of the mandibular fossa. Trigger points in this muscle refer pain into the temporal mandibular joint and maxillary sinus. Trigger points in this muscle are often the cause of pain felt from TMJ dysfunction.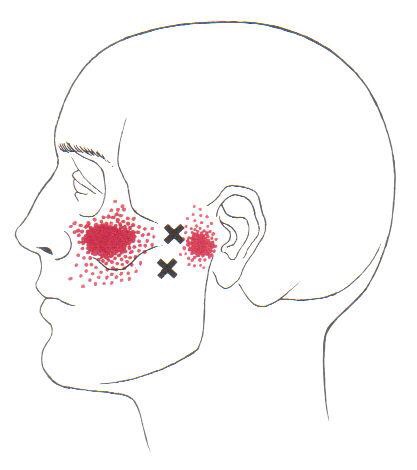
5 Tips for Safe Leaf Raking this Fall

It’s that time of year again. Those colorful leaves falling from the trees will soon leave you with a big mess on the lawn and a new chore to add to your to-do list. Before grabbing the rake, take these tips into consideration to avoid the soreness and injury that commonly accompany leaf raking.
1. Stretch
It may not seem like a workout, but leaf raking can be a very strenuous activity, especially if you’re not regularly active already. Be sure to do a quick warm-up to get your muscles ready and stretch to limit soreness in your neck, shoulders, and back.
2. Use the Right Equipment
Make sure you’re using a rake that’s the correct size for your height. A rake that’s too small will cause you to bend over more often and put more stress on your back. Wear gloves to protect your palms.
3. Use Correct Posture
Keep your back straight and upright. You’ll want to bend at the knees – not the waist – when picking up your piles and always avoid twisting your torso.
4. Switch Arms Often
Avoid an overuse injury with your dominant arm by switching sides frequently.
5. Take Breaks
Remember to give yourself a little recovery time now and then and stay hydrated. Taking frequent breaks will help you avoid exhaustion and strain.
As with any form of physical activity, listen to your body. Any sudden, sharp, or persistent pain is not normal. Stay safe by following these tips and be sure to give our office a call if you experience any neck, shoulder, or back pain this fall.
2 Critical Steps to Resolving Ankle Sprains
Efficient treatment of ankle sprains continues well after the pain subsides. While the majority of inversion (lateral) ankle sprains heal relatively quickly, up to 1/3 of patients, continue to note symptoms at one year, and up to 25% report pain, instability, crepitus, weakness, stiffness, or swelling at three years. (1) Re-injury is frequent, with rates reaching almost 75% in sports, like basketball. (2) Successful management of ankle sprains and prevention of re-injury are predicated on a couple of fundamental principles.
Management of ankle inversion sprains requires two steps; each is equally important.
- The first step entails the evaluation and treatment of acute pain.
- The second step involves preventing subsequent sprains – and new research validates the importance of chiropractic care to improve clinical outcomes in these recalcitrant cases.
STEP 1—Move for Pain Relief
Early return to activity for acute inversion sprains is supported by the literature. Exercises and treatments that promote joint motion and early return to weight bearing for acute ankle sprains have proven more effective than immobilization. While grade III sprains (ligament rupture) may require immobilization, grade I and II ankle sprains should forego complete immobilization and instead focus on regaining full range of motion. In fact, early rehab and return to weight bearing will increase ankle range of motion, decrease pain, and reduce swelling sooner than immobilization.
In a study by Linde et al., 150 patients with inversion ankle sprains were treated with early motion and weight bearing. After one month, 90% of the patients treated with early motion and weight bearing demonstrated pain-free gait and 97% had increased work ability. (3) Early mobility exercises would typically include:
These four exercises promote balance and range of motion – specifically dorsiflexion, which is a key contributor to ankle injury. Patients who have lost an average of 11 degrees of dorsiflexion are five times more likely to suffer lateral ankle sprains. (4)
In office care should also include mobilization and manipulation for restoring function. Joint mobilization has been shown to decrease pain, increase dorsiflexion, and improve ankle function. (5) IASTM or transverse friction massage to the affected ligament may help mobilize scar tissue and increase pliability. Myofascial release may help release tightness or adhesions in the gastroc and soleus. (Side note: The FAKTR concept seamlessly incorporates all of these tools to produce top-tier outcomes.)
Knowing when to treat and when to refer is critical. Whitman’s clinical prediction rule identifies four variables to predict the success of manipulation and exercise for the treatment of inversion ankle sprains. (6) The presence of three out of four of the following variables predict greater than a 95% success rate for manual therapy and exercise:
- Symptoms worse when standing
- Symptoms worse in the evening
- Navicular drop greater than 5 mm
- Distal tibiofibular joint hypomobility
STEP 2- Prevent Re-injury
The second step is shorter and easier than the first. The most crucial variable in the successful prevention of future ankle sprains is improving BALANCE. Balance training reduces the incidence of ankle sprains and increases dynamic neuromuscular control, postural sway, and joint position sense in athletes. (7) A study by de Vasconcelos et al. (2018) found that balance training reduced the incidence of ankle sprains by 38% compared with the control group. (7)
Two of the most common exercises used for balance and proprioception include the single-leg stance exercise and Veles. A simple explanation stressing the importance of balance training may be necessary to promote patient compliance.
Finally, encourage your patients start walking “normal” as soon as possible. As evidence-based chiropractors, we need to return patients back to their normal gait as soon as tolerable. Patients with foot and ankle pain will often favor a supinated gait in order to unload the soft tissues of the foot and arch in favor of their bony architecture on the lateral foot. The lateral column of the foot affords stability but at the expense of a very inefficient gait. Over an extended period, these patients may develop a Tailor’s bunion, i.e. 5th metatarsal head bursitis. However, in the case of ankle sprains, a rapid increase in activity may overload the metatarsal fast enough to cause a Jones Fracture. Return to normal gait will minimize these compensations.
A treatment with Bryan Cobb RMT.
Session Description
A treatment with Bryan is very user friendly. And, no, you don’t have to remove any clothing. However, bringing a t-shirt and a pair of shorts or sweats is recommended.
The first time you come for a treatment you will be asked to fill out a Client History form. Bryan will go over the information you provide, asking for more detail and discussing the type of pain you are having and its location.
The treatment itself involves locating the Trigger Points in the muscle or soft tissue and applying a deep focused pressure to the Point. This will reproduce the pain and the referral pattern that is characteristic of that pain.
The treatment will be uncomfortable at first, but as the Trigger Points release, the pain will decrease. The pressure will always be adjusted to your tolerance level. If, at any time, you feel too uncomfortable you can ask Bryan to ease off a bit.
Depending on your specific problem, Bryan may also use some stretching and / or range-of-motion techniques, as needed.
After treatment, it is usually recommended that the client apply moist heat to the area treated.
What the Heck Is a Trigger Point?
By Bryan Cobb, Advanced Remedial Massage Therapist
What is a Trigger Point?
Trigger Points (TP’s) are defined as a “hyper-irritable spot within a taut band of skeletal muscle. The spot is painful on compression and can evoke characteristic referred pain and autonomic phenomena.”1
Put into plain language, a TP is a painful knot in muscle tissue that can refer pain to other areas of the body. You have probably felt the characteristic achy pain and stiffness that TP’s produce, at some time in your life.
TP’s were first brought to the attention of the medical world by Dr. Janet G. Travell. Dr. Travell, physician to President John F. Kennedy, is the acknowledged Mother of Myofascial Trigger Points. In fact, “Trigger Point massage, the most effective modality used by massage therapists for the relief of pain, is based almost entirely on Dr. Travell’s insights.”2 Dr. Travell’s partner in her research was Dr. David G. Simons, a research scientist and aerospace physician.
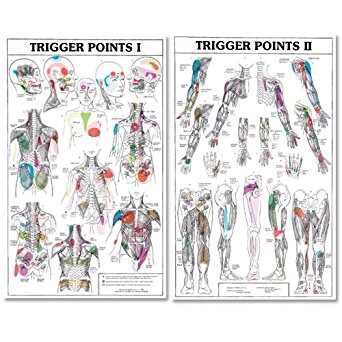
Trigger Points are very common. In fact, Travell and Simons state that TP’s are responsible for, or associated with, 75% of pain complaints or conditions.1 With this kind of prevalence, it’s no wonder that TP’s are often referred to as the “scourge of mankind”.
Trigger Points can produce a wide variety of pain complaints. Some of the most common are migraine headaches, back pain, and pain and tingling into the extremities. They are usually responsible for most cases of achy deep pain that is hard to localize.
A TP will refer pain in a predictable pattern, based on its location in a given muscle. Also, since these spots are bundles of contracted muscle fibres, they can cause stiffness and a decreased range of motion. Chronic conditions with many TP’s can also cause general fatigue and malaise, as well as muscle weakness.
Trigger Points are remarkably easy to get, but the most common causes are
•
TP’s (black dots) can refer pain to other areas (red)

Sudden overload of a muscle
• Poor posture
• Chronic frozen posture (e.g., from a desk job), and
• Repetitive strain
Once in place, a TP can remain there for the remainder of your life unless an intervention takes place.
Trigger Points Not Well Known
With thousands of people dealing with chronic pain, and with TP’s being responsible for — or associated with — a high percentage of chronic pain, it is very disappointing to find that a large portion of doctors and other health care practitioners don’t know about TP’s and their symptoms.
Scientific research on TP’s dates back to the 1700’s. There are numerous medical texts and papers written on the subject.
But, it still has been largely overlooked by the health care field. This has led to needless frustration and suffering, as well as thousands of lost work hours and a poorer quality of life.
How Are Trigger Points Treated?
As nasty and troublesome as TP’s are, the treatment for them is surely straight-forward. A skilled practitioner will assess the individual’s pain complaint to determine the most likely location of the TP’s and then apply one of several therapeutic modalities, the most effective of which is a massage technique called “ischemic compression”.
Basically, the therapist will apply a firm, steady pressure to the TP, strong enough to reproduce the symptoms. The pressure will remain until the tissue softens and then the pressure will increase appropriately until the next barrier is felt. This pressure is continued until the referral pain has subsided and the TP is released. (Note: a full release of TP’s could take several sessions.)
Other effective modalities include dry needling (needle placed into the belly of the TP) or wet needling (injection into the TP). The use of moist heat and stretching prove effective, as well. The best practitioners for TP release are Massage Therapists, Physiotherapists, and Athletic Therapists. An educated individual can also apply ischemic compression to themselves, but should start out seeing one of the above therapists to become familiar with
the modality and how to apply pressure safely.
1 Simons, D.G., Travell, D.G., & Simons, L.S. Travell and Simons’ Myofascial Pain and Dysfunction: the Trigger Point Manual.
Vol. 1. 2nd ed. Lippincott, Williams, and Wilkins, 1999.
2http://www.muscletherapyworks.com/MTW%20Biography%20T%20&%20S%2001.htm
Trigger points in the deltoid muscle
The deltoid is the main muscle that makes up the shoulder. It originates on the clavicle, acromion, and spine of the scapula. It inserts on the deltoid tuberosity of the humerus. The deltoid acts at the shoulder to produce abduction, and assist with flexion and extension. The deltoid is especially prone to developing trigger points. These posterior style will refer pain into the anterior and lateral shoulder. Trigger points in the posterior delt will refer pain into the posterior shoulder with spillover down the lateral arm.