Winnipeg
Plantar Fasciitis and Laser Therapy
What is it?
Plantar fasciitis is inflammation of the thick tissue on the bottom of the foot that connects the heel to the toes and creates the arch of the foot.
Symptoms
The most common complaint is pain in the bottom of the heel. The heel pain may be dull or sharp. The bottom of the foot may also ache or burn. This can be painful and make walking more difficult.
The pain is usually worse:
- In the morning when you take your first steps
- After standing or sitting for a while
- When climbing stairs
- After intense activity
The pain may develop slowly over time, or suddenly after intense activity.
What Causes Plantar Fasciitis?
Plantar fasciitis develops because of repeated small tears to the flat band of ligamentous tissue that connects your heel to the bones of your toes. These tears weaken the arch that supports the foot. As the arch of the foot weakens, increasing strain is placed on the deeper ligaments and tendons of the foot and lower leg. Over time, Plantar Fasciitis can result in Chronic Pain, Heel Spurs and Degenerative Joint Disease (Arthritis).
You are more likely to get plantar fasciitis if you have:
• Foot arch problems (both flat feet and high arches)
• Long-distance running, especially running downhill or on uneven surfaces
• Sudden weight gain or obesity
• Tight Achilles tendon (the tendon connecting the calf muscles to the heel)
• Shoes with poor arch support or soft soles
Plantar fasciitis is seen in both men and women. However, it most often affects active men ages 40 – 70. It is one of the most common orthopedic complaints relating to the foot.
Plantar fasciitis is commonly thought of as being caused by a heel spur, but research has found that this is not the case. On x-ray, heel spurs are seen in people with and without plantar fasciitis.
Signs and tests
The health care provider will perform a physical exam. This may show:
• Tenderness on the bottom of your foot
• Flat feet or high arches
• Mild foot swelling or redness
• Stiffness or tightness of the arch in the bottom of your foot.
Physicians typically treat Plantar Fasciitis with anti-inflammatory drugs and steroid injections. These medications temporarily reduce the pain associated with Plantar Fasciitis but do not treat the cause of the problem. Traditional methods can usually take between 9 months to two years to resolve this condition.
Class IV Laser Plantar Fasciitis Program
Our program utilizes the latest class IV Lasers, and combines them with other therapies to help reduce the pain, strengthen the muscles around the foot and ankle joints, and increase range of motion. The Class IV Laser is at the heart of our treatment program. It provides a safe, effective, non-invasive, painless solution for plantar fasciitis. Patients generally respond exceptionally well to treatments and usually notice significant pain relief after just a few treatments.
Permanent correction of Plantar Fasciitis requires two procedures.
1. Heal the Damaged Fascia
Ending the pain caused by Plantar Fasciitis requires stopping the cycle of inflammation. This is critical because chronically inflamed tissues block the flow of needed nutrients and oxygen to surrounding muscles and joints. The advanced CLASS IV LASER restores the flow of nutrients and oxygen to the inflamed tissue allowing the cells to repair themselves at an accelerated rate.
2. Correct the Foot and Gait Mechanics
Most cases of plantar fasciitis are resolved very easily with Class IV Laser Therapy alone; however, if the condition has become chronic this can lead to alterations in the gait that will have to be addressed. This could involve stabilizing the arch with orthotics or implementing a simple series of specific strengthening and stretching exercises.
Plantar fasciitis when treated early has an exceptionally good prognosis with our protocol. We encourage those with Plantar Fasciitis to seek our help right away. The longer one suffers with this painful condition the more likely it will cause other conditions in the knee, hip and spine.
Relieve Tension Headaches with Chiropractic Care: A Natural Solution


Tension headaches are a common ailment that many people experience at some point in their lives. Characterized by a dull, aching pain and a feeling of tightness or pressure across the forehead, sides, or back of the head, tension headaches can significantly impact daily life. While over-the-counter medications can provide temporary relief, chiropractic care offers a natural, non-invasive solution to address the root causes of tension headaches and provide lasting relief.
Understanding Tension Headaches
Tension headaches, also known as stress headaches, are typically caused by muscle contractions in the head and neck regions. These contractions can be triggered by various factors, including:
- Stress: Emotional stress can cause muscle tension, leading to headaches.
- Poor Posture: Sitting or standing for long periods with improper posture can strain neck and shoulder muscles.
- Muscle Strain: Overuse of the muscles in the neck and shoulders, often due to repetitive activities, can lead to tension headaches.
- Eye Strain: Extended screen time or reading without breaks can cause eye and muscle strain.
- Fatigue: Lack of sleep and general fatigue can contribute to muscle tension and headaches.
How Chiropractic Care Can Help
Chiropractic care focuses on diagnosing and treating musculoskeletal disorders, particularly those involving the spine. Chiropractors use a variety of techniques to help relieve tension headaches by addressing their underlying causes. Here are some ways chiropractic care can benefit those suffering from tension headaches:
- Spinal Adjustments:
- Spinal adjustments, or manipulations, help correct misalignments in the spine. These misalignments can cause muscle tension and nerve irritation, contributing to headaches. By realigning the spine, chiropractors can reduce tension and improve overall spinal health.
- Muscle Relaxation:
- Chiropractors use various techniques, such as massage, trigger point therapy, and myofascial release, to relax tight muscles in the neck and shoulders. These treatments help reduce muscle tension and improve blood flow, alleviating headache symptoms.
- Posture Correction:
- Poor posture is a common cause of tension headaches. Chiropractors assess your posture and provide guidance on how to maintain proper alignment throughout the day. They may recommend ergonomic changes at work or home to reduce strain on your muscles.
- Stress Management:
- Stress is a significant trigger for tension headaches. Chiropractors often provide advice on stress management techniques, such as relaxation exercises, mindfulness, and breathing exercises, to help reduce overall stress levels and prevent headaches.
- Exercise and Stretching:
- Regular exercise and stretching can help maintain muscle flexibility and strength, reducing the likelihood of tension headaches. Chiropractors can develop personalized exercise and stretching routines to address your specific needs.
- Lifestyle and Nutritional Advice:
- Chiropractors offer holistic care, which includes advice on lifestyle and nutrition. They may suggest dietary changes or supplements to support overall health and reduce headache frequency.
Benefits of Chiropractic Care for Tension Headaches
Opting for chiropractic care to manage tension headaches comes with several benefits:
- Natural and Non-Invasive: Chiropractic care provides a drug-free, non-surgical approach to headache relief.
- Addresses Root Causes: Instead of just masking symptoms, chiropractic treatments aim to address the underlying causes of tension headaches.
- Improves Overall Health: Chiropractic care not only helps with headaches but also promotes overall spinal health and well-being.
- Reduces Reliance on Medication: Regular chiropractic treatments can reduce the need for over-the-counter or prescription pain medications.
- Enhances Quality of Life: With reduced headache frequency and severity, you can enjoy a better quality of life and improved daily functioning.
River East Chiropractic: Your Partner in Headache Relief
At River East Chiropractic, we understand how debilitating tension headaches can be. Our experienced chiropractors are dedicated to helping you find relief through personalized, comprehensive care. Our facility offers a range of services, including chiropractic care, acupuncture, massage, occupational therapy, Pilates, and a full gym. Our holistic approach ensures that all aspects of your health are addressed to provide lasting relief from tension headaches.
Don’t let tension headaches control your life. Visit River East Chiropractic today and discover how our natural, effective treatments can help you achieve a headache-free life. Our team is here to support you every step of the way, ensuring you stay healthy, active, and pain-free.
Happy Halloween!
Be careful out there on the roads tonight! Kids are everywhere!

What is Whiplash?

Whiplash is an injury to the soft-tissues of the neck often referred to as a sprain or strain. Because there are a unique set of symptoms associated with whiplash, doctors and researchers commonly use the term “whiplash associated disorders” or WAD to describe the condition.
WAD commonly occurs as a result of a car crash, but it can also result from a slip and fall, sports injury, a personal injury (such as an assault), and other traumatic causes. The tissues commonly involved include muscle tendons (“strain”), ligaments and joint capsules (“sprains”), disk injuries (tears, herniation), as well as brain injury or concussion—even without hitting the head!
Symptoms vary widely but often include neck pain, stiffness, tender muscles and connective tissue (myofascial pain), headache, dizziness, sensations such as burning, prickly, tingling, numbness, muscle weakness, and referred pain to the shoulder blade, mid-back, arm, head, or face. If concussion occurs, additional symptoms include cognitive problems, concentration loss, poor memory, anxiety/depression, nervousness/irritability, sleep disturbance, fatigue, and more!
Whiplash associated disorders can be broken down into three categories: WAD I includes symptoms without any significant examination findings; WAD II includes loss of cervical range of motion and evidence of soft-tissue damage; and WAD III includes WAD II elements with neurological loss—altered motor and/or sensory functions. There is a WAD IV which includes fracture, but this is less common and often excluded.
Treatment for WAD includes everything from doing nothing to intensive management from multiple disciplines—chiropractic, primary care, physical therapy, clinical psychology, pain management, and specialty services such as neurology, orthopedics, and more. The goal of treatment is to restore normal function and activity participation, as well as symptom management.
The prognosis of WAD is generally good as many will recover without residual problems within days to weeks, with most people recovering around three months after the injury. Unfortunately, some are not so lucky and have continued neck pain, stiffness, headache, and some develop post-concussive syndrome. The latter can affect cognition, memory, vision, and other brain functions. Generally speaking, the higher the WAD category, the worse the prognosis, although each case MUST be managed by its own unique characteristics. If the injury includes neurological loss (muscle strength and/or sensory dysfunction like numbness, tingling, burning, pressure), the prognosis is often worse.
Chiropractic care for the WAD patient can include manipulation, mobilization, and home-based exercises, as well as the use of anti-inflammatory herbs (ginger, turmeric, proteolysis enzymes (bromelain, papain), devil’s claw, boswellia extract, rutin, bioflavonoid, vitamin D, coenzyme Q10, etc.) and dietary modifications aimed at reducing inflammation and promoting healing.
* 83% of those patients involved in an MVA will suffer whiplash injury and 50% will be symptomatic at 1 year.
* 90% of patients with neurologic signs at onset may be symptomatic at 1 year.
* 25- 80% of patients who suffer a whiplash injury will experience late-onset dizziness
* Clinicians should be observant for radiographic signs of instability, including interspinous widening, vertebral subluxation, vertebral compression fracture, and loss of cervical lordosis.
* Horizontal displacement of greater than 3.5 mm or angular displacement of more than 11 degrees on flexion/extension views suggests instability
Whiplash and Your Posture

Posture assessment is a key component of the chiropractic examination, and the posture of the head and neck is especially important for a patient recovering from a whiplash injury. Forward head carriage describes a state in which the head sits more forward on the shoulders than it should. In order for the muscles in the neck and shoulders to keep the head upright, they must work harder. This added strain can increase one’s risk for neck pain and headaches, which is why retraining posture is a key component to the management of neck pain and headaches in patients with or without a history of whiplash.
Forward head carriage also increases the distance between the back of the head and the headrest in the seated position, especially when the seat is reclined. In a rear-end collision, a gap greater than a half an inch between the head rest and the back of the head increases the probability of injury due to the greater distance the head can hyperextend as it rebounds backwards into the headrest. This makes posture correction of forward head carriage an important aspect of treatment from both a preventative and curative perspective.
So this begs the question, can forward head carriage be corrected? The simple answer is “yes!” One study evaluated the effects of a 16-week resistance and stretching program designed to address forward head posture and protracted shoulder positioning.
Researchers conducted the study in two separate secondary schools with 130 adolescents aged 15–17 years with forward head and protracted shoulder posture. The control group participated in a regular physical education (PE) program while the experimental group attended the same PE classes with the addition of specific exercises for posture correction. The research ream measured the teens’ shoulder head posture from the side using two different validated methods and tracked symptoms using a questionnaire. The results revealed a significant improvement in the shoulder and cervical angle in the experimental group that did not occur in the control group.
The conclusion of the study strongly supports that a 16-week resistance and stretching program is effective in decreasing forward head and protracted shoulder posture in adolescents. This would suggest that a program such as this should be strongly considered in the regular curriculum of PE courses since this is such a common problem.
Doctors of chiropractic are trained to evaluate and manage forward head posture with shoulder protraction. This can prove beneficial in both the prevention as well as management of signs and symptoms associated with a whiplash injury.
What Causes Low Back Pain?
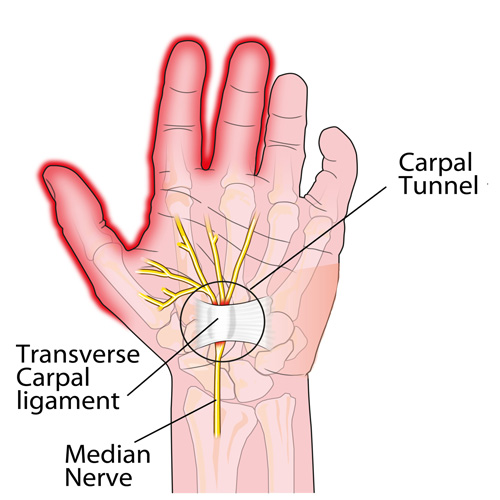
Carpal Tunnel Syndrome #3

This week, we will conclude our three-part series on important facts regarding carpal tunnel syndrome (CTS).
CTS TREATMENT OPTIONS (continued): Aside from the carpal tunnel, there are several places where the median nerve can become compressed as it travels from the neck, down through the shoulder, through tight muscular areas of the upper arm and forearm, and finally through the carpal tunnel at the wrist. In order to achieve good, long-lasting results, treatment must focus on relieving compression at any point along the course of the nerve. This is why chiropractic works SO WELL as it addresses ALL of these areas using manual adjustments, muscle release techniques, and even physical therapy modalities.
CTS PREVENTION: Because there are multiple causes of CTS, prevention must be tailored to each person. For example, if the patient has diabetes mellitus, maintaining a proper blood sugar level is very important because the blood becomes thicker as the sugar levels increase and it simply cannot pass through our small blood vessels (capillaries), especially those located in the feet and hands. This can eventually lead to the need for amputation due to poor circulation and contribute to the numbness associated with diabetic neuropathy.
Similarly, low thyroid function results in a type of swelling called myxedema that can cause or worsen CTS, and keeping the thyroid hormone balanced in the bloodstream is very important. Managing other conditions that create inflammation or swelling, such as rheumatoid and other types of arthritis, will also help prevent CTS from developing or worsening.
Carpal tunnel syndrome can also occur during pregnancy due to the hormonal shifts similar for those taking birth control pills. The PRICE treatment options presented last month can be very helpful for the pregnant mother and represent important non-medication self-care approaches.
Certain occupations that require fast, repetitive work and/or firm gripping can result in carpal tunnel syndrome because of the friction that results in swelling that occurs when the muscle tendons inside the carpal tunnel rub excessively fast together (kind of like starting a fire with two sticks). Modifying the work task until the swelling is controlled is VERY important, as discussed last month.
Other preventative measures include exercises that keep the muscles and tendons in the forearm and inside the carpal tunnel stretched so that the tendons easily slide inside their respective muscle tendon sheaths. This is accomplished by placing the palm side of the hand (elbow straight) on a wall with the fingers pointing downwards while reaching across with the opposite hand and pulling the thumb back until you feel a good firm stretch. Hold this position for 5-10 seconds or until the forearm muscles feel like they are relaxing. Repeat this multiple times a day.
We realize you have a choice in whom you consider for your health care provision and we sincerely appreciate your trust in choosing our service for those needs. If you, a friend, or family member requires care for Carpal Tunnel Syndrome, we would be honored to render our services.
Do I have a tension headache? Or Migranes?


Most likely, everyone reading this article has had a headache at one time or another. The American Headache Society reports that nearly 40% of the population suffers from episodic headaches each year while 3% have chronic tension-type headaches. The United States Department of Health and Human Services estimates that 29.5 million Americans experience migraines, but tension headaches are more common than migraines at a frequency of 5 to 1. Knowing the difference between the two is important, as the proper diagnosis can guide treatment in the right direction.
TENSION HEADACHES: These typically result in a steady ache and tightness located in the neck, particularly at the base of the skull, which can irritate the upper cervical nerve roots resulting in radiating pain and/or numbness into the head. At times, the pain can reach the eyes but often stops at the top of the head. Common triggers include stress, muscle strain, or anxiety.
MIGRAINE HEADACHES: Migraines are often much more intense, severe, and sometimes incapacitating. They usually remain on one side of the head and are associated with nausea and/or vomiting. An “aura”, or a pre-headache warning, often comes with symptoms such as a bright flashing light, ringing or noise in the ears, a visual floater, and more. For migraine headaches, there is often a strong family history, which indicates genetics may play a role in their origin.
There are many causes for headaches. Commonly, they include lack of sleep and/or stress and they can also result from a recent injury—such as a car accident, and/or a sports injury—especially when accompanied by a concussion.
Certain things can “trigger” a migraine including caffeine, chocolate, citrus fruits, cured meats, dehydration, depression, diet (skipping meals), dried fish, dried fruit, exercise (excessive), eyestrain, fatigue (extreme), food additives (nitrites, nitrates, MSG), lights (bright, flickering, glare), menstruation, some medications, noise, nuts, odors, onions, altered sleep, stress, watching TV, red wine/alcohol, weather, etc.
Posture is also a very important consideration. A forward head carriage is not only related to headaches, but also neck and back pain. We’ve previously pointed out that every inch (2.54 cm) the average 12 pound head (5.44 kg) shifts forwards adds an EXTRA ten pounds (4.5 kg) of load on the neck and upper back muscles to keep the head upright.
So, what can be done for people who suffer from headaches? First, research shows chiropractic care is highly effective for patients with both types of headaches. Spinal manipulation, deep tissue release techniques, and nutritional counseling are common approaches utilized by chiropractors. Patients are also advised to use some of these self-management strategies at home as part of their treatment plan: the use of ice, self-trigger point therapy, exercise (especially strengthening the deep neck flexors), and nutritional supplements.
What Exercises Should I Do For Fibro?

Fibromyalgia (FM) is a very common, chronic condition where the patient describes “widespread pain” not limited to one area of the body. Hence, when addressing exercises for FM, one must consider the whole body. Perhaps one of the most important to consider is the squat.
If you think about it, we must squat every time we sit down, stand up, get in/out of our car, and in/out of bed. Even climbing and descending steps results in a squat-lunge type of movement.
The problem with squatting is that we frequently lose (or misuse) the proper way to do this when we’re in pain as the pain forces us to compensate, which can cause us to develop faulty movement patterns that can irritate our ankles, knees, hips, and spine (particularly the low back). In fact, performing a squatting exercise properly will strengthen the hips, which will help protect the spine, and also strengthens the glutel muscles, which can help you perform all the daily activities mentioned above.
The “BEST” type of squat is the free-standing squat. This is done by bending the ankles, knees, and hips while keeping a curve in the low back. The latter is accomplished by “…sticking the butt out” during the squat.
Do NOT allow the knees to drift beyond your toes! If you notice sounds coming from your knees they can be ignored IF they are not accompanied by pain. If you do have pain, try moving the foot of the painful knee about six inches (~15 cm) ahead of the other and don’t squat as far down. Move within “reasonable boundaries of pain” by staying away from positions that reproduce sharp, lancinating pain that lingers upon completion.