Between 80% and 90% of the general population will experience an episode of lower back pain (LBP) at least once during their lives. When it affects the young to middle-aged, we often use the term “non-specific LBP” to describe the condition. The geriatric population suffers from the “aging effects” of the spine—things like degenerative joint disease, degenerative disk disease, and spinal stenosis. Fractures caused by osteoporosis can also result in back pain.
Physio
My Hip Hurts….

One of the structures that is frequently blamed for hip pain is called the labrum—the rubbery tissue that surrounds the socket helping to stabilize the hip joint. This tissue often wears and tears with age, but it can also be torn as a result of a trauma or sports-related injury.
The clinical significance of a labral tear of the hip is controversial, as these can be found in people who don’t have any pain at all. We know from studies of the intervertebral disks located in the lower back that disk herniation is often found in pain-free subjects—between 20-50% of the normal population. In other words, the presence of abnormalities on an MRI is often poorly associated with patient symptoms, and the presence of a labral tear of the hip appears to be quite similar.
For instance, in a study of 45 volunteers (average age 38, range: 15–66 years old; 60% males) with no history of hip pain, symptoms, injury, or prior surgery, MRIs reviewed by three board-certified radiologists revealed a total of 73% of the hips had abnormalities, of which more than two-thirds were labral tears.
Another interesting study found an equal number of labral tears in a group of professional ballet dancers (both with and without hip pain) and in non-dancer control subjects of similar age and gender.
Another study showed that diagnostic blocks—a pain killer injected into the hip for diagnostic purposes to determine if it’s a pain generator—failed to offer relief for those with labral tears.
Doctors of chiropractic are trained to identify the origins of pain arising from the low back, pelvis, hip, and knee, all of which can mimic or produce hip symptoms. Utilizing information derived from a careful history, examination, imaging (when appropriate), and functional tests, chiropractors can offer a nonsurgical, noninvasive, safe method of managing hip pain.
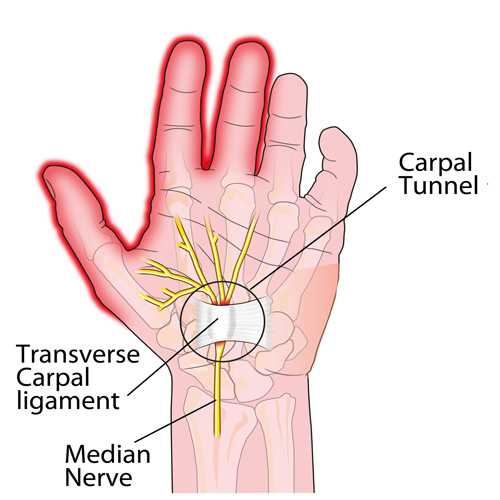
Carpel Tunnel in a nutshell
Here it is: carpal tunnel syndrome (CTS) in a nutshell!
Condition Of The Month: Thoracic Joint Restriction

Your spine is made up of 24 bones stacked on top of each other with a soft “disc” between each segment to allow for flexibility. Normally, each joint in your spine should move freely and independently. When one or more of your spinal vertebra is slightly misaligned and restricted, we call this condition a “spinal segmental joint restriction”. A “thoracic joint restriction” means that this misalignment or restriction is located in your upper or mid-back region.
To help visualize this, imagine a normal spine functioning like a big spring moving freely in every direction. A spine with a joint restriction is like having a section of that spring welded together. The spring may still move as a whole, but a portion of it is no longer functioning.
Joint restrictions can develop in many ways. Sometimes they are brought on by an accident or an injury. Other times, they develop from repetitive strains or poor posture. Being overweight, smoking, strenuous work, and emotional stress can make you more susceptible to problems.
Restricted joints give rise to a self-perpetuating cycle of discomfort. Joint restriction causes swelling and inflammation, which triggers muscular guarding leading to more restriction. Since your spine functions as a unit, rather than as isolated pieces, a joint restriction in one area of your spine often causes “compensatory” problems in another. Think of this as a rowboat with multiple oarsmen on each side. When one rower quits, the others are placed under additional stress and can become overworked.
Joint restrictions most commonly cause local tenderness and discomfort. You may notice that your range of motion is limited. Movement may increase your discomfort. Pain from a restricted joint often trickles around your rib cage or up & down your spine. Be sure to tell your chiropractor if your symptoms include any chest pain, shortness of breath, unusual cough, indigestion or flu- like complaints.
Long-standing restrictions are thought to result in arthritis – much like the way a slightly misaligned wheel on your car causes premature wearing of your tire.
You should recognize that your problem is common and generally treatable. Chiropractic care has been shown to be the safest and most effective treatment for joint restrictions. Our office offers several tools to help ease your pain. To speed your recovery, you should avoid activities that increase your pain. Be sure to take frequent breaks from sedentary activity. Yoga has been shown to help back pain sufferers so consider joining a class or picking up a DVD.
Pregnancy and Low Back Pain?

What is CTS?
What is Whiplash?

Whiplash is an injury to the soft-tissues of the neck often referred to as a sprain or strain. Because there are a unique set of symptoms associated with whiplash, doctors and researchers commonly use the term “whiplash associated disorders” or WAD to describe the condition.
WAD commonly occurs as a result of a car crash, but it can also result from a slip and fall, sports injury, a personal injury (such as an assault), and other traumatic causes. The tissues commonly involved include muscle tendons (“strain”), ligaments and joint capsules (“sprains”), disk injuries (tears, herniation), as well as brain injury or concussion—even without hitting the head!
Symptoms vary widely but often include neck pain, stiffness, tender muscles and connective tissue (myofascial pain), headache, dizziness, sensations such as burning, prickly, tingling, numbness, muscle weakness, and referred pain to the shoulder blade, mid-back, arm, head, or face. If concussion occurs, additional symptoms include cognitive problems, concentration loss, poor memory, anxiety/depression, nervousness/irritability, sleep disturbance, fatigue, and more!
Whiplash associated disorders can be broken down into three categories: WAD I includes symptoms without any significant examination findings; WAD II includes loss of cervical range of motion and evidence of soft-tissue damage; and WAD III includes WAD II elements with neurological loss—altered motor and/or sensory functions. There is a WAD IV which includes fracture, but this is less common and often excluded.
Treatment for WAD includes everything from doing nothing to intensive management from multiple disciplines—chiropractic, primary care, physical therapy, clinical psychology, pain management, and specialty services such as neurology, orthopedics, and more. The goal of treatment is to restore normal function and activity participation, as well as symptom management.
The prognosis of WAD is generally good as many will recover without residual problems within days to weeks, with most people recovering around three months after the injury. Unfortunately, some are not so lucky and have continued neck pain, stiffness, headache, and some develop post-concussive syndrome. The latter can affect cognition, memory, vision, and other brain functions. Generally speaking, the higher the WAD category, the worse the prognosis, although each case MUST be managed by its own unique characteristics. If the injury includes neurological loss (muscle strength and/or sensory dysfunction like numbness, tingling, burning, pressure), the prognosis is often worse.
Chiropractic care for the WAD patient can include manipulation, mobilization, and home-based exercises, as well as the use of anti-inflammatory herbs (ginger, turmeric, proteolysis enzymes (bromelain, papain), devil’s claw, boswellia extract, rutin, bioflavonoid, vitamin D, coenzyme Q10, etc.) and dietary modifications aimed at reducing inflammation and promoting healing.
* 83% of those patients involved in an MVA will suffer whiplash injury and 50% will be symptomatic at 1 year.
* 90% of patients with neurologic signs at onset may be symptomatic at 1 year.
* 25- 80% of patients who suffer a whiplash injury will experience late-onset dizziness
* Clinicians should be observant for radiographic signs of instability, including interspinous widening, vertebral subluxation, vertebral compression fracture, and loss of cervical lordosis.
* Horizontal displacement of greater than 3.5 mm or angular displacement of more than 11 degrees on flexion/extension views suggests instability.
Why Does My Back Hurt?

PFPS Cont. You want details?

The muscles of the hip provide not only local stability, but also play an important role in spinal and lower extremity functional alignment. (1-4) While weakness in some hip muscles (hip extensors and knee extensors) is well tolerated, weakness or imbalance in others can have a profound effect on gait and biomechanical function throughout the lower half of the body. (5) Weakness of the hip abductors, particularly those that assist with external rotation, has the most significant impact on hip and lower extremity stability. (5,6)
The gluteus medius is the principal hip abductor. When the hip is flexed, the muscle also assists the six deep hip external rotators (piriformis, gemelli, obturators, and quadratus femoris). The gluteus medius originates on the ilium just inferior to the iliac crest and inserts on the lateral and superior aspects of the greater trochanter. While the principal declared action of the gluteus medius is hip abduction, clinicians will appreciate its more valuable contribution as a dynamic stabilizer of the hip and pelvis- particularly during single leg stance activities like walking, running, and squatting. The gluteus medius contributes approximately 70% of the abduction force required to maintain pelvic leveling during single leg stance. The remainder comes predominantly from 2 muscles that insert onto the iliotibial band: the tensor fascia lata and upper gluteus maximus. Hip abductor strength is the single greatest contributor to lower extremity frontal plain alignment during activity. (6)

Incompetent hip abductors and/or external rotators allows for excessive adduction and internal rotation of the thigh during single leg stance activities. This leads to a cascade of biomechanical problems, including pelvic drop, excessive hip adduction, excessive femoral internal rotation, valgus knee stress, and internal tibial rotation. (1,7-12)
References
1. Szu-Ping Lee, Powers C. Description of a Weight-Bearing Method to Assess Hip Abductor and External Rotator Muscle Performance. JOSPT. Volume 43, Issue 6
2. Crossley KM, Zhang WJ, Schache AG, Bryant A, Cowan SM. Performance on the single-leg squat task indicates hip abductor muscle function. Am J Sports Med. 2011;39:866-873.
3. Presswood L, Cronin J, Keogh JWL, Whatman C. Gluteus medius: applied anatomy, dysfunction, assessment, and progressive strengthening. Strength Cond J. 2008;30:41-53.
4. Sled EA, Khoja L, Deluzio KJ, Olney SJ, Culham EG. Effect of a home program of hip abductor ex- ercises on knee joint loading, strength, function, and pain in people with knee osteoarthritis: a clinical trial. Phys Ther. 2010;90:895-904.
5. van der Krogt MM, Delp SL, Schwartz MH How robust is human gait to muscle weakness? Gait Posture. 2012 Feb 29.
6. Laurie Stickler, Margaret Finley, Heather Gulgin Relationship between hip and core strength and frontal plane alignment during a single leg squat Physical Therapy in Sport Available online 2 June 2014
7. Ireland ML, Willson JD, Ballantyne BT, Davis
IM. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003;33:671-676.
8. Noehren B, Davis I, Hamill J. ASB clinical biome- chanics award winner 2006: prospective study of the biomechanical factors associated with iliotib- ial band syndrome. Clin Biomech (Bristol, Avon). 2007;22:951-956.
9. Powers CM. The influence of abnormal hip me- chanics on knee injury: a biomechanical perspec- tive. J Orthop Sports Phys Ther. 2010;40:42-51.
10. Powers CM. The influence of altered lower- extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33:639-646.
11. Sigward SM, Powers CM. Loading characteristics of females exhibiting excessive valgus moments during cutting. Clin Biomech (Bristol, Avon). 2007;22:827-833
12. Souza RB, Powers CM. Differences in hip kine- matics, muscle strength, and muscle activation between subjects with and without patellofemo- ral pain. J Orthop Sports Phys Ther. 2009;39:12- 19.
Patellofemoral Pain Syndrome
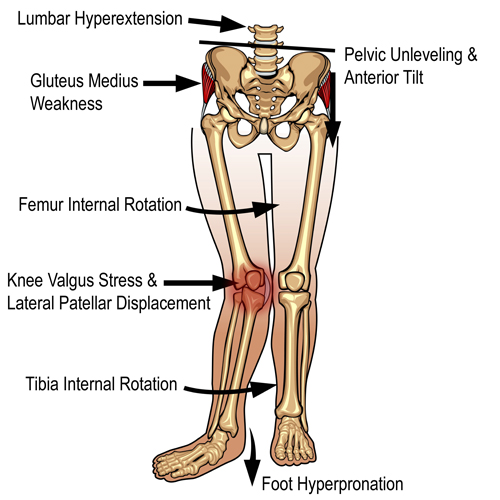
Patellofemoral pain syndrome (PFPS), also called “Runners Knee”, describes the symptom complex of knee discomfort, swelling, or crepitus that results from excessive or imbalanced forces acting on the joint. It is the most common cause of knee pain in the general population, affecting an estimated 25% of adults.
PFPS is most commonly related to lateral tracking of the patella. The patella has a natural tendency to migrate laterally due to the pull of the quadriceps and the slight natural valgus of the lower extremity. A new study in the Journal of Sports Medicine (1) provides additional confirmation that when managing patellofemoral pain syndrome, clinicians must address two critical yet often overlooked issues.
This study concludes that PFPS and dynamic knee valgus do not arise primarily from knee dysfunction, rather from hip abductor/ external rotator weakness and/or foot hyperpronation.
“The most effective intervention programs included exercises targeting the hip external rotator and abductor muscles and knee extensor muscles.” and “PFPS patients with foot abnormalities, such as those with increased rearfoot eversion or pes pronatus, may benefit the most from foot orthotics.”
Since gluteus medius and VMO weakness are key factors in the development of PFPS, strengthening exercises that target those muscles prove most effective. Stabilization exercises may include pillow push (push the back of your knee into a pillow for 5-6 seconds), supine heel slide, terminal knee (short-arc) extension, clam, glut bridge, semi-stiff deadlift, posterior lunge, and monster walk.
Myofascial release and stretching should be directed at hypertonic muscles, including the TFL, gastroc, soleus, hamstring, piriformis, hip rotators, and psoas. Myofascial release or IASTM may be appropriate for tightness in the iliotibial band, vastus lateralis, posterior hip capsule, and lateral knee retinaculum.
Manipulation may be necessary for restrictions in the lumbosacral and lower extremity joints. Hypermobility is common in the ipsilateral SI joint with restrictions present contralaterally. Evidence has shown that patellar tracking braces, i.e. BioSkin® or PatellaPro®, may lead to better outcomes.
Lifestyle modification may be necessary to reduce pain-provoking endeavors, especially running, jumping and other activities that induce a valgus stress. Athletes should avoid allowing their knee to cross in front of their toes while squatting. Arch supports or custom orthotics may be necessary to correct hyperpronation. Runners should avoid cross-over gaits and change shoes every 250 to 500 miles.
.
.
.
.
.
.
.
#pain
#kneepain
#chiropractic
#fitness
#sports
#wellness
#fitness
#healthyliving
#healthychoices
#Winnipeg
References
1. Petersen W, Rembitzki I, Liebau C. Patellofemoral pain in athletes. Open Access Journal of Sports Medicine. 2017;8:143-15