Be careful out there on the roads tonight! Kids are everywhere!

Be careful out there on the roads tonight! Kids are everywhere!


Whiplash is an injury to the soft-tissues of the neck often referred to as a sprain or strain. Because there are a unique set of symptoms associated with whiplash, doctors and researchers commonly use the term “whiplash associated disorders” or WAD to describe the condition.
WAD commonly occurs as a result of a car crash, but it can also result from a slip and fall, sports injury, a personal injury (such as an assault), and other traumatic causes. The tissues commonly involved include muscle tendons (“strain”), ligaments and joint capsules (“sprains”), disk injuries (tears, herniation), as well as brain injury or concussion—even without hitting the head!
Symptoms vary widely but often include neck pain, stiffness, tender muscles and connective tissue (myofascial pain), headache, dizziness, sensations such as burning, prickly, tingling, numbness, muscle weakness, and referred pain to the shoulder blade, mid-back, arm, head, or face. If concussion occurs, additional symptoms include cognitive problems, concentration loss, poor memory, anxiety/depression, nervousness/irritability, sleep disturbance, fatigue, and more!
Whiplash associated disorders can be broken down into three categories: WAD I includes symptoms without any significant examination findings; WAD II includes loss of cervical range of motion and evidence of soft-tissue damage; and WAD III includes WAD II elements with neurological loss—altered motor and/or sensory functions. There is a WAD IV which includes fracture, but this is less common and often excluded.
Treatment for WAD includes everything from doing nothing to intensive management from multiple disciplines—chiropractic, primary care, physical therapy, clinical psychology, pain management, and specialty services such as neurology, orthopedics, and more. The goal of treatment is to restore normal function and activity participation, as well as symptom management.
The prognosis of WAD is generally good as many will recover without residual problems within days to weeks, with most people recovering around three months after the injury. Unfortunately, some are not so lucky and have continued neck pain, stiffness, headache, and some develop post-concussive syndrome. The latter can affect cognition, memory, vision, and other brain functions. Generally speaking, the higher the WAD category, the worse the prognosis, although each case MUST be managed by its own unique characteristics. If the injury includes neurological loss (muscle strength and/or sensory dysfunction like numbness, tingling, burning, pressure), the prognosis is often worse.
Chiropractic care for the WAD patient can include manipulation, mobilization, and home-based exercises, as well as the use of anti-inflammatory herbs (ginger, turmeric, proteolysis enzymes (bromelain, papain), devil’s claw, boswellia extract, rutin, bioflavonoid, vitamin D, coenzyme Q10, etc.) and dietary modifications aimed at reducing inflammation and promoting healing.
* 83% of those patients involved in an MVA will suffer whiplash injury and 50% will be symptomatic at 1 year.
* 90% of patients with neurologic signs at onset may be symptomatic at 1 year.
* 25- 80% of patients who suffer a whiplash injury will experience late-onset dizziness
* Clinicians should be observant for radiographic signs of instability, including interspinous widening, vertebral subluxation, vertebral compression fracture, and loss of cervical lordosis.
* Horizontal displacement of greater than 3.5 mm or angular displacement of more than 11 degrees on flexion/extension views suggests instability

Posture assessment is a key component of the chiropractic examination, and the posture of the head and neck is especially important for a patient recovering from a whiplash injury. Forward head carriage describes a state in which the head sits more forward on the shoulders than it should. In order for the muscles in the neck and shoulders to keep the head upright, they must work harder. This added strain can increase one’s risk for neck pain and headaches, which is why retraining posture is a key component to the management of neck pain and headaches in patients with or without a history of whiplash.
Forward head carriage also increases the distance between the back of the head and the headrest in the seated position, especially when the seat is reclined. In a rear-end collision, a gap greater than a half an inch between the head rest and the back of the head increases the probability of injury due to the greater distance the head can hyperextend as it rebounds backwards into the headrest. This makes posture correction of forward head carriage an important aspect of treatment from both a preventative and curative perspective.
So this begs the question, can forward head carriage be corrected? The simple answer is “yes!” One study evaluated the effects of a 16-week resistance and stretching program designed to address forward head posture and protracted shoulder positioning.
Researchers conducted the study in two separate secondary schools with 130 adolescents aged 15–17 years with forward head and protracted shoulder posture. The control group participated in a regular physical education (PE) program while the experimental group attended the same PE classes with the addition of specific exercises for posture correction. The research ream measured the teens’ shoulder head posture from the side using two different validated methods and tracked symptoms using a questionnaire. The results revealed a significant improvement in the shoulder and cervical angle in the experimental group that did not occur in the control group.
The conclusion of the study strongly supports that a 16-week resistance and stretching program is effective in decreasing forward head and protracted shoulder posture in adolescents. This would suggest that a program such as this should be strongly considered in the regular curriculum of PE courses since this is such a common problem.
Doctors of chiropractic are trained to evaluate and manage forward head posture with shoulder protraction. This can prove beneficial in both the prevention as well as management of signs and symptoms associated with a whiplash injury.

A great injury prevention movement is the glute-ham raise. Done after a warm up and prior to competition it will significantly reduce the odds of hamstring strains in running athletes in sports like Soccer, Football and Sprinting.
To perform the movement:
Begin in a tall kneeling position on a cushion or pillow.
Partner grabs and holds ankles to ground or hook your feet under a stable surface.
Keeping your torso neutral and your thighs in line with your body, bend forward at the knees, using your hamstrings to control the speed of your forward bend.
Go as far as you can without cramping, pain or falling to the ground.

Your spine is made up of 24 bones stacked on top of each other with a soft “disc” between each segment to allow for flexibility. Normally, each joint in your spine should move freely and independently. When one or more of your spinal vertebra is slightly misaligned and restricted, we call this condition a “spinal segmental joint restriction”. A “thoracic joint restriction” means that this misalignment or restriction is located in your upper or mid-back region.
To help visualize this, imagine a normal spine functioning like a big spring moving freely in every direction. A spine with a joint restriction is like having a section of that spring welded together. The spring may still move as a whole, but a portion of it is no longer functioning.
Joint restrictions can develop in many ways. Sometimes they are brought on by an accident or an injury. Other times, they develop from repetitive strains or poor posture. Being overweight, smoking, strenuous work, and emotional stress can make you more susceptible to problems.
Restricted joints give rise to a self-perpetuating cycle of discomfort. Joint restriction causes swelling and inflammation, which triggers muscular guarding leading to more restriction. Since your spine functions as a unit, rather than as isolated pieces, a joint restriction in one area of your spine often causes “compensatory” problems in another. Think of this as a rowboat with multiple oarsmen on each side. When one rower quits, the others are placed under additional stress and can become overworked.
Joint restrictions most commonly cause local tenderness and discomfort. You may notice that your range of motion is limited. Movement may increase your discomfort. Pain from a restricted joint often trickles around your rib cage or up & down your spine. Be sure to tell your chiropractor if your symptoms include any chest pain, shortness of breath, unusual cough, indigestion or flu- like complaints.
Long-standing restrictions are thought to result in arthritis – much like the way a slightly misaligned wheel on your car causes premature wearing of your tire.
You should recognize that your problem is common and generally treatable. Chiropractic care has been shown to be the safest and most effective treatment for joint restrictions. Our office offers several tools to help ease your pain. To speed your recovery, you should avoid activities that increase your pain. Be sure to take frequent breaks from sedentary activity. Yoga has been shown to help back pain sufferers so consider joining a class or picking up a DVD.
Whiplash is an injury to the soft-tissues of the neck often referred to as a sprain or strain. Because there are a unique set of symptoms associated with whiplash, doctors and researchers commonly use the term “whiplash associated disorders” or WAD to describe the condition.
WAD commonly occurs as a result of a car crash, but it can also result from a slip and fall, sports injury, a personal injury (such as an assault), and other traumatic causes. The tissues commonly involved include muscle tendons (“strain”), ligaments and joint capsules (“sprains”), disk injuries (tears, herniation), as well as brain injury or concussion—even without hitting the head!
Symptoms vary widely but often include neck pain, stiffness, tender muscles and connective tissue (myofascial pain), headache, dizziness, sensations such as burning, prickly, tingling, numbness, muscle weakness, and referred pain to the shoulder blade, mid-back, arm, head, or face. If concussion occurs, additional symptoms include cognitive problems, concentration loss, poor memory, anxiety/depression, nervousness/irritability, sleep disturbance, fatigue, and more!
Whiplash associated disorders can be broken down into three categories: WAD I includes symptoms without any significant examination findings; WAD II includes loss of cervical range of motion and evidence of soft-tissue damage; and WAD III includes WAD II elements with neurological loss—altered motor and/or sensory functions. There is a WAD IV which includes fracture, but this is less common and often excluded.
Treatment for WAD includes everything from doing nothing to intensive management from multiple disciplines—chiropractic, primary care, physical therapy, clinical psychology, pain management, and specialty services such as neurology, orthopedics, and more. The goal of treatment is to restore normal function and activity participation, as well as symptom management.
The prognosis of WAD is generally good as many will recover without residual problems within days to weeks, with most people recovering around three months after the injury. Unfortunately, some are not so lucky and have continued neck pain, stiffness, headache, and some develop post-concussive syndrome. The latter can affect cognition, memory, vision, and other brain functions. Generally speaking, the higher the WAD category, the worse the prognosis, although each case MUST be managed by its own unique characteristics. If the injury includes neurological loss (muscle strength and/or sensory dysfunction like numbness, tingling, burning, pressure), the prognosis is often worse.
Chiropractic care for the WAD patient can include manipulation, mobilization, and home-based exercises, as well as the use of anti-inflammatory herbs (ginger, turmeric, proteolysis enzymes (bromelain, papain), devil’s claw, boswellia extract, rutin, bioflavonoid, vitamin D, coenzyme Q10, etc.) and dietary modifications aimed at reducing inflammation and promoting healing.
* 83% of those patients involved in an MVA will suffer whiplash injury and 50% will be symptomatic at 1 year.
* 90% of patients with neurologic signs at onset may be symptomatic at 1 year.
* 25- 80% of patients who suffer a whiplash injury will experience late-onset dizziness
* Clinicians should be observant for radiographic signs of instability, including interspinous widening, vertebral subluxation, vertebral compression fracture, and loss of cervical lordosis.
* Horizontal displacement of greater than 3.5 mm or angular displacement of more than 11 degrees on flexion/extension views suggests instability.

The muscles of the hip provide not only local stability, but also play an important role in spinal and lower extremity functional alignment. (1-4) While weakness in some hip muscles (hip extensors and knee extensors) is well tolerated, weakness or imbalance in others can have a profound effect on gait and biomechanical function throughout the lower half of the body. (5) Weakness of the hip abductors, particularly those that assist with external rotation, has the most significant impact on hip and lower extremity stability. (5,6)
The gluteus medius is the principal hip abductor. When the hip is flexed, the muscle also assists the six deep hip external rotators (piriformis, gemelli, obturators, and quadratus femoris). The gluteus medius originates on the ilium just inferior to the iliac crest and inserts on the lateral and superior aspects of the greater trochanter. While the principal declared action of the gluteus medius is hip abduction, clinicians will appreciate its more valuable contribution as a dynamic stabilizer of the hip and pelvis- particularly during single leg stance activities like walking, running, and squatting. The gluteus medius contributes approximately 70% of the abduction force required to maintain pelvic leveling during single leg stance. The remainder comes predominantly from 2 muscles that insert onto the iliotibial band: the tensor fascia lata and upper gluteus maximus. Hip abductor strength is the single greatest contributor to lower extremity frontal plain alignment during activity. (6)
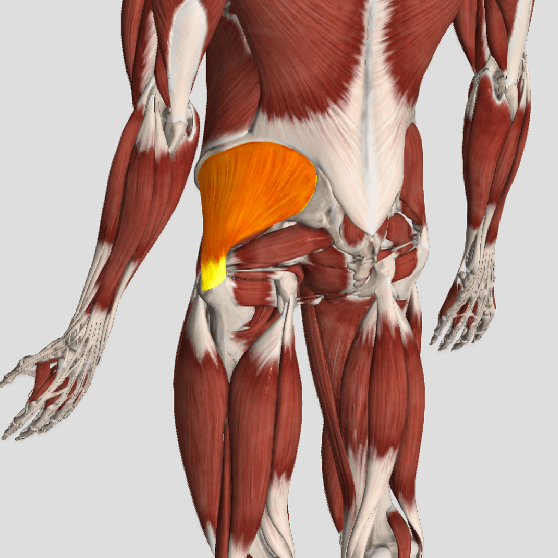
Incompetent hip abductors and/or external rotators allows for excessive adduction and internal rotation of the thigh during single leg stance activities. This leads to a cascade of biomechanical problems, including pelvic drop, excessive hip adduction, excessive femoral internal rotation, valgus knee stress, and internal tibial rotation. (1,7-12)

Exercise: Yoga Gaining in Popularity in the United States.
Over the past decade, yoga has experienced a notable surge in popularity, with a remarkable uptick in participation observed across diverse age groups. According to data compiled by the National Center for Health Statistics in February 2015, the percentage of adults engaging in yoga has more than doubled, soaring from just under 6% in 2002 to over 10% in 2012. This trend is mirrored among children and seniors, reflecting a widespread recognition of yoga’s myriad benefits for physical, mental, and emotional well-being.
At its core, yoga is far more than a mere physical exercise regimen; it embodies an ancient tradition rooted in the harmonization of body, mind, and spirit. Through a synthesis of mindful movement, controlled breathing, and meditation, yoga fosters a profound sense of inner peace, serenity, and interconnectedness with the world around us. Its holistic approach to health and wellness transcends the confines of conventional fitness routines, offering practitioners a pathway to holistic flourishing and self-discovery.
For adults, yoga serves as a sanctuary from the stresses of modern life, providing a sanctuary where they can reconnect with themselves and cultivate resilience in the face of adversity. Meanwhile, children benefit from the developmental advantages conferred by yoga, including improved concentration, enhanced flexibility, and heightened emotional intelligence. For seniors, yoga offers a gentle yet effective means of maintaining mobility, alleviating chronic pain, and fostering a sense of vitality and vitality in their golden years.
As yoga continues to captivate hearts and minds worldwide, its transformative potential as a catalyst for personal growth and well-being remains undeniable. By embracing yoga as a holistic lifestyle practice, individuals of all ages can embark on a journey of self-discovery, healing, and empowerment, enriching their lives immeasurably in the process.