Back Pain
“Other” Causes of Low Back Pain
Between 80% and 90% of the general population will experience an episode of lower back pain (LBP) at least once during their lives. When it affects the young to middle-aged, we often use the term “non-specific LBP” to describe the condition. The geriatric population suffers from the “aging effects” of the spine—things like degenerative joint disease, degenerative disk disease, and spinal stenosis. Fractures caused by osteoporosis can also result in back pain.
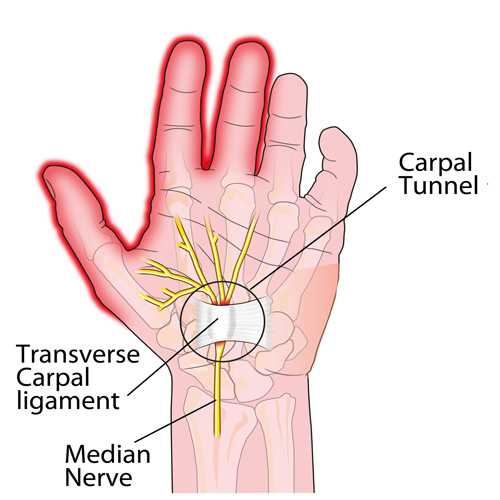
Carpel Tunnel in a nutshell
Here it is: carpal tunnel syndrome (CTS) in a nutshell!
Condition Of The Month: Thoracic Joint Restriction

Your spine is made up of 24 bones stacked on top of each other with a soft “disc” between each segment to allow for flexibility. Normally, each joint in your spine should move freely and independently. When one or more of your spinal vertebra is slightly misaligned and restricted, we call this condition a “spinal segmental joint restriction”. A “thoracic joint restriction” means that this misalignment or restriction is located in your upper or mid-back region.
To help visualize this, imagine a normal spine functioning like a big spring moving freely in every direction. A spine with a joint restriction is like having a section of that spring welded together. The spring may still move as a whole, but a portion of it is no longer functioning.
Joint restrictions can develop in many ways. Sometimes they are brought on by an accident or an injury. Other times, they develop from repetitive strains or poor posture. Being overweight, smoking, strenuous work, and emotional stress can make you more susceptible to problems.
Restricted joints give rise to a self-perpetuating cycle of discomfort. Joint restriction causes swelling and inflammation, which triggers muscular guarding leading to more restriction. Since your spine functions as a unit, rather than as isolated pieces, a joint restriction in one area of your spine often causes “compensatory” problems in another. Think of this as a rowboat with multiple oarsmen on each side. When one rower quits, the others are placed under additional stress and can become overworked.
Joint restrictions most commonly cause local tenderness and discomfort. You may notice that your range of motion is limited. Movement may increase your discomfort. Pain from a restricted joint often trickles around your rib cage or up & down your spine. Be sure to tell your chiropractor if your symptoms include any chest pain, shortness of breath, unusual cough, indigestion or flu- like complaints.
Long-standing restrictions are thought to result in arthritis – much like the way a slightly misaligned wheel on your car causes premature wearing of your tire.
You should recognize that your problem is common and generally treatable. Chiropractic care has been shown to be the safest and most effective treatment for joint restrictions. Our office offers several tools to help ease your pain. To speed your recovery, you should avoid activities that increase your pain. Be sure to take frequent breaks from sedentary activity. Yoga has been shown to help back pain sufferers so consider joining a class or picking up a DVD.
Pregnancy and Low Back Pain?

River East Chiropractic: Your Local Wellness Hub

Welcome to River East Chiropractic at 1187 Rothesay St!
We’re thrilled to introduce our new health and wellness clinic at 1187 Rothesay Street, right here in your neighbourhood. Whether you’re seeking pain relief, stress reduction, or a customized fitness plan, we’ve got you covered with a wide range of services designed to enhance your well-being.
Our Services
Here’s what you can expect when you visit us:
- Chiropractic Care: Our skilled chiropractors provide effective treatments for back pain, headaches, sports injuries, and more. Let us help you get back to feeling your best.
- Acupuncture: Whether you’re looking to relieve pain, reduce stress, or improve your overall health, our acupuncture services offer a natural and time-tested solution.
- Laser Therapy: Using advanced technology, our low-level laser therapy speeds up healing and reduces pain, particularly for conditions like arthritis, soft tissue injuries, and chronic pain.
- Gym & Personal Training: Our on-site gym offers top-notch equipment and personalized fitness plans from our experienced trainers to help you reach your health and fitness goals.
- Free Child Care During Treatment: We understand how challenging it can be to focus on your health with little ones in tow, so we offer free child care while you receive treatment.
- Massage Therapy: Soothe your aching muscles with our RMT
Convenient Hours for Your Busy Schedule
We know that life can be hectic, which is why we offer evening appointments until 8pm on Mondays and Thursdays to fit your schedule. Plus, we’re open from 9 AM to 1 PM on Saturdays to make it easier for you to prioritize your health.
Get in Touch
We’d love to welcome you to River East Chiropractic! For more information or to book an appointment, visit us online at rivereastchiropractic.ca or give us a call at (204) 334-3334. Your journey to better health starts here.
Why Does My Back Hurt?

PFPS Cont. You want details?

The muscles of the hip provide not only local stability, but also play an important role in spinal and lower extremity functional alignment. (1-4) While weakness in some hip muscles (hip extensors and knee extensors) is well tolerated, weakness or imbalance in others can have a profound effect on gait and biomechanical function throughout the lower half of the body. (5) Weakness of the hip abductors, particularly those that assist with external rotation, has the most significant impact on hip and lower extremity stability. (5,6)
The gluteus medius is the principal hip abductor. When the hip is flexed, the muscle also assists the six deep hip external rotators (piriformis, gemelli, obturators, and quadratus femoris). The gluteus medius originates on the ilium just inferior to the iliac crest and inserts on the lateral and superior aspects of the greater trochanter. While the principal declared action of the gluteus medius is hip abduction, clinicians will appreciate its more valuable contribution as a dynamic stabilizer of the hip and pelvis- particularly during single leg stance activities like walking, running, and squatting. The gluteus medius contributes approximately 70% of the abduction force required to maintain pelvic leveling during single leg stance. The remainder comes predominantly from 2 muscles that insert onto the iliotibial band: the tensor fascia lata and upper gluteus maximus. Hip abductor strength is the single greatest contributor to lower extremity frontal plain alignment during activity. (6)

Incompetent hip abductors and/or external rotators allows for excessive adduction and internal rotation of the thigh during single leg stance activities. This leads to a cascade of biomechanical problems, including pelvic drop, excessive hip adduction, excessive femoral internal rotation, valgus knee stress, and internal tibial rotation. (1,7-12)
References
1. Szu-Ping Lee, Powers C. Description of a Weight-Bearing Method to Assess Hip Abductor and External Rotator Muscle Performance. JOSPT. Volume 43, Issue 6
2. Crossley KM, Zhang WJ, Schache AG, Bryant A, Cowan SM. Performance on the single-leg squat task indicates hip abductor muscle function. Am J Sports Med. 2011;39:866-873.
3. Presswood L, Cronin J, Keogh JWL, Whatman C. Gluteus medius: applied anatomy, dysfunction, assessment, and progressive strengthening. Strength Cond J. 2008;30:41-53.
4. Sled EA, Khoja L, Deluzio KJ, Olney SJ, Culham EG. Effect of a home program of hip abductor ex- ercises on knee joint loading, strength, function, and pain in people with knee osteoarthritis: a clinical trial. Phys Ther. 2010;90:895-904.
5. van der Krogt MM, Delp SL, Schwartz MH How robust is human gait to muscle weakness? Gait Posture. 2012 Feb 29.
6. Laurie Stickler, Margaret Finley, Heather Gulgin Relationship between hip and core strength and frontal plane alignment during a single leg squat Physical Therapy in Sport Available online 2 June 2014
7. Ireland ML, Willson JD, Ballantyne BT, Davis
IM. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003;33:671-676.
8. Noehren B, Davis I, Hamill J. ASB clinical biome- chanics award winner 2006: prospective study of the biomechanical factors associated with iliotib- ial band syndrome. Clin Biomech (Bristol, Avon). 2007;22:951-956.
9. Powers CM. The influence of abnormal hip me- chanics on knee injury: a biomechanical perspec- tive. J Orthop Sports Phys Ther. 2010;40:42-51.
10. Powers CM. The influence of altered lower- extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33:639-646.
11. Sigward SM, Powers CM. Loading characteristics of females exhibiting excessive valgus moments during cutting. Clin Biomech (Bristol, Avon). 2007;22:827-833
12. Souza RB, Powers CM. Differences in hip kine- matics, muscle strength, and muscle activation between subjects with and without patellofemo- ral pain. J Orthop Sports Phys Ther. 2009;39:12- 19.
Exercise Helps LBP!

Moving is good for your back and muscles, especially if you have back pain.
The Interplay of Pain and Mobility in Elderly Fall Risk

Chiropractic: Chronic Pain May Increase Fall Risk for Seniors!
The ramifications of falls among elderly individuals extend far beyond the physical injury itself, often encroaching upon independence and diminishing overall quality of life. Traditionally, impaired motor function has been pinpointed as a primary risk factor for falls among the elderly. However, a recent report published in Aging Clinical and Experimental Research in March 2015 has unveiled a startling revelation: older adults with ostensibly normal motor function are not immune to the perils of falls, particularly when grappling with chronic musculoskeletal pain across multiple body sites.
This finding challenges conventional wisdom and underscores the intricate interplay between pain and mobility in the context of fall risk among the elderly. Chronic musculoskeletal pain, pervasive among aging populations, introduces a formidable obstacle to mobility and stability, predisposing individuals to the hazards of falls despite outwardly intact motor function.
The implications of this report reverberate throughout the realms of geriatric healthcare and fall prevention. Healthcare providers must adopt a holistic approach to fall risk assessment, incorporating not only measures of motor function but also comprehensive evaluations of pain and musculoskeletal health. By identifying and addressing chronic pain as a modifiable risk factor, clinicians can mitigate the likelihood of falls and safeguard the independence and well-being of elderly patients.
Furthermore, this research underscores the imperative for multidisciplinary interventions aimed at enhancing mobility, managing pain, and fortifying musculoskeletal health among aging populations. Through targeted strategies encompassing physical therapy, pain management, and lifestyle modifications, healthcare professionals can empower older adults to navigate their golden years with confidence and vitality, minimizing the specter of falls and preserving their autonomy and quality of life.